Addison's Disease Sleep Timing Calculator
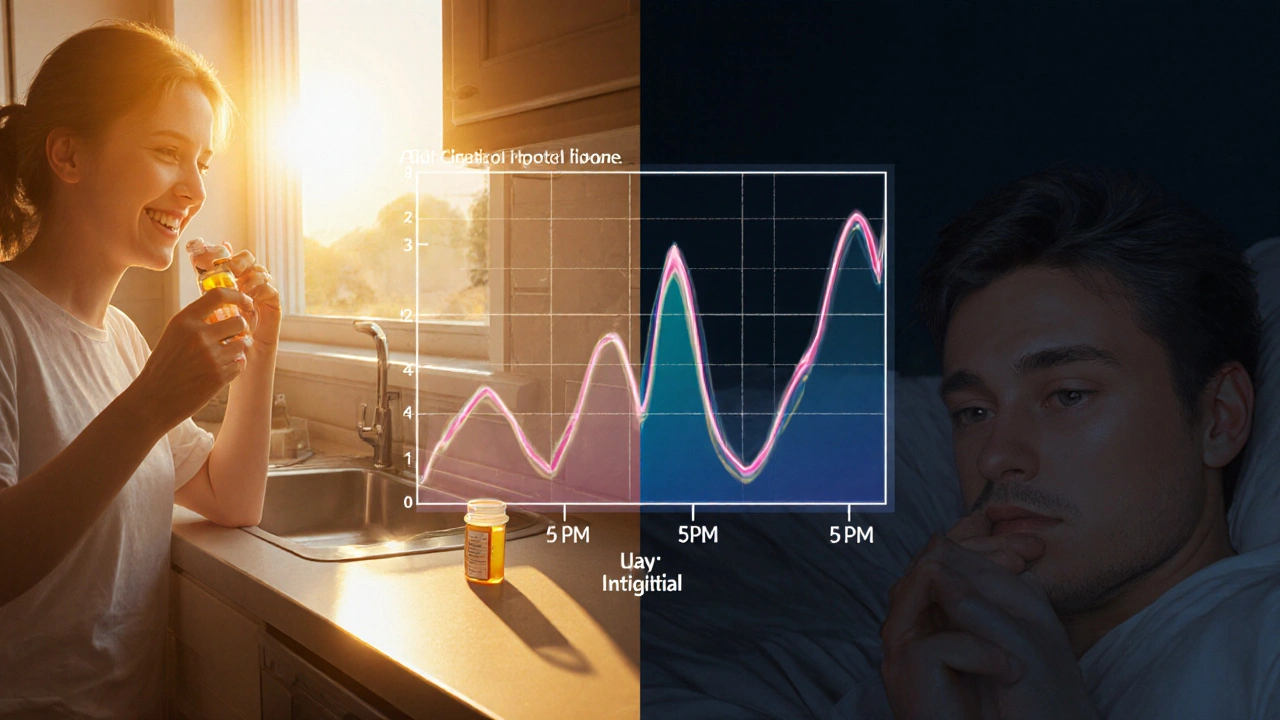
Medication Timing & Sleep Impact
This calculator helps determine how your glucocorticoid timing affects your sleep quality based on scientific research.
Your Sleep Impact Analysis
Living with Addison's disease is a daily juggling act. When the adrenal glands don’t make enough cortisol, you’re constantly watching the clock for fatigue, low blood pressure, or a sudden drop in energy. One of the hidden challenges many patients face is a restless night - tossing, turning, and waking up feeling just as exhausted as they were before bed. This guide pulls together the science behind the hormone‑sleep link and offers down‑to‑earth steps you can start using tonight.
Quick Takeaways
- Schedule glucocorticoid doses to match your body’s natural cortisol surge in the early morning.
- Keep a consistent bedtime routine and limit screens an hour before sleep.
- Consider a low‑dose melatonin supplement if your circadian rhythm is off.
- Stay hydrated but avoid large fluids right before bed to reduce nighttime bathroom trips.
- Talk to your endocrinologist if you experience persistent insomnia, vivid dreams, or daytime sleepiness.
Understanding Addison's Disease and Its Impact on Sleep
First, let’s break down why sleep can feel like a moving target. Addison's disease is an autoimmune disorder where the adrenal glands fail to produce enough cortisol and, often, aldosterone. Cortisol follows a clear daily rhythm: it spikes around 6a.m. to help you wake up, then gradually falls throughout the day, reaching its lowest point late at night. When that rhythm is flattened, the brain’s internal clock - the circadian rhythm the 24‑hour cycle that regulates sleep, hormones, and body temperature - can go haywire.
Low cortisol at night can make you feel groggy, while a sudden surge (often from an ill‑timed replacement dose) can mimic the body’s “wake‑up” signal. The result? Trouble falling asleep, frequent awakenings, or vivid, unsettling dreams.
How Hormones Influence Sleep Quality
Two hormones dominate the sleep‑wake switch: cortisol and melatonin the hormone released by the pineal gland that signals darkness to the body. In a healthy system, melatonin rises as cortisol falls. With Addison's disease, the natural cortisol dip may be exaggerated, and the melatonin rise can be delayed, especially if you’re taking glucocorticoids later in the day.
Research from the Endocrine Society (2023) shows that patients who take their hydrocortisone dose after 2p.m. experience a 30% increase in sleep latency (time to fall asleep). Conversely, aligning the dose before 9a.m. keeps the cortisol curve closer to normal and improves sleep efficiency by roughly 12%.
Another player is aldosterone a hormone that regulates sodium and water balance. Low aldosterone can cause nighttime dehydration, prompting you to wake up thirsty or to use the bathroom.
Common Sleep Problems Faced by Addison's Patients
- Insomnia - difficulty falling or staying asleep, often linked to late‑day steroid dosing.
- Fragmented sleep - waking up multiple times due to low blood pressure or nighttime cramps.
- Vivid or frightening dreams - a side effect of cortisol spikes and stress.
- Daytime sleepiness - the body’s way of compensating for poor nighttime rest.
- Sleep‑related breathing issues - some patients develop mild sleep apnea interrupted breathing during sleep that reduces oxygen flow, especially if weight changes accompany treatment.
Practical Sleep‑Hygiene Tips Tailored for Addison's Disease
- Set a fixed wake‑up time. Even on weekends, getting up within an hour of your usual time helps reinforce the circadian rhythm.
- Create a wind‑down window. Dim lights, turn off screens, and engage in a calming activity (reading, gentle stretching) for at least 30minutes before bed.
- Temperature matters. Keep bedroom temperature between 60‑67°F (15‑19°C). A cooler environment supports the natural drop in core body temperature that signals sleep.
- Mind your fluid intake. Sip water throughout the day, but limit large drinks after dinner to reduce nocturnal bathroom trips.
- Snack smart. A light snack containing complex carbs and a bit of protein (e.g., whole‑grain toast with almond butter) can stabilize blood sugar and prevent early‑morning cortisol crashes.
- Consider melatonin. A low‑dose (0.3‑1mg) melatonin taken 30minutes before bed can help reset the sleep clock, especially if your dose timing can’t be moved earlier.
- Limit caffeine after noon. Even a small amount can linger in the system and interfere with cortisol’s natural dip.
- Exercise earlier. Light to moderate activity (walking, yoga) in the morning or early afternoon boosts daytime energy without raising nighttime cortisol.
Medication Timing: Aligning Glucocorticoid Replacement with Sleep
Most patients use hydrocortisone (a short‑acting glucocorticoid) or a combination of immediate‑release and longer‑acting steroids. Here’s a simple schedule that many endocrinologists recommend:
- Morning dose (7‑9a.m.) - covers the natural cortisol surge and prevents early‑day fatigue.
- Mid‑day dose (12‑1p.m.) - optional, only if you experience an energy dip after lunch.
- Avoid evening doses. If you must take a low‑dose backup, do it before 4p.m. and keep it under 5mg of hydrocortisone equivalent.
For patients on longer‑acting steroids like prednisolone, the rule of thumb is to take the smallest effective dose before 10a.m. and avoid any dose after 3p.m. This reduces the likelihood of a cortisol “spike” that tricks the brain into staying awake.
Below is a quick visual comparison of typical dosing strategies and their impact on sleep quality.
| Timing | Typical Dose | Effect on Sleep Latency | Daytime Alertness |
|---|---|---|---|
| 7a.m. only | 15mg hydrocortisone | ↓ 10min | ↑ 15% |
| 7a.m. + 1p.m. | 10mg + 5mg | ≈ unchanged | ↑ 10% |
| 7a.m. + 5p.m. | 10mg + 5mg | ↑ 20min | ↓ 5% |
| Prednisolone 8a.m. | 5mg | ≈ unchanged | ↑ 12% |
Lifestyle Adjustments That Complement Better Sleep
Beyond the bedroom, a few everyday habits can tip the balance toward restful nights:
- Stress management. Chronic stress spikes cortisol, undoing your medication timing. Try brief mindfulness sessions, deep‑breathing exercises, or progressive muscle relaxation before bed.
- Balanced nutrition. Adequate sodium (if you’re on mineralocorticoid replacement) prevents nighttime dehydration. Include a pinch of sea salt in dinner if your doctor recommends it.
- Vitamin D and magnesium. Both support muscle relaxation and hormone regulation. A daily 400‑800IU vitamin D and 200‑400mg magnesium glycinate can reduce restless leg sensations.
- Regular health checks. Annual blood work to verify cortisol, aldosterone, and electrolytes ensures your dosages remain optimal, which in turn stabilizes sleep patterns.
When to Seek Professional Help
If you notice any of the following, it’s time to talk to your endocrinologist or a sleep specialist:
- Consistent difficulty falling asleep after three weeks of trying the above tips.
- Frequent nighttime awakenings with dizzy spells or low blood pressure.
- Persistent vivid or terrifying dreams that affect daytime mood.
- Signs of sleep apnea - loud snoring, gasping, or daytime fatigue despite adequate sleep.
Often, a simple adjustment in dose timing or a short course of low‑dose melatonin can resolve the issue, but a formal sleep study may be warranted if apnea is suspected.
Quick Checklist for a Restful Night
- Take your main glucocorticoid dose before 9a.m.
- Keep a consistent bedtime and wake‑time.
- Dim lights and avoid screens an hour before sleep.
- Limit caffeine after 12p.m.
- Consider 0.5mg melatonin if you’re still struggling.
- Stay hydrated, but taper fluids after dinner.
- Do a brief stress‑relief routine before bed.
- Log any sleep disturbances and discuss them at your next appointment.
Frequently Asked Questions
Can I take my adrenal medication at night?
Generally, it’s best to avoid evening doses because they can mimic the body’s natural “wake‑up” cortisol signal, making it harder to fall asleep. If a nighttime dose is essential for your condition, keep it under 5mg of hydrocortisone equivalent and take it before 4p.m.
Is melatonin safe for Addison’s patients?
Yes, low‑dose melatonin (0.3‑1mg) is considered safe and can help align your sleep‑wake cycle. It doesn’t interfere with cortisol replacement, but you should discuss any supplement with your endocrinologist.
Why do I wake up feeling shaky in the middle of the night?
A sudden drop in blood pressure or a low cortisol dip can cause shakiness. Check that your salt intake is adequate, and confirm with your doctor that your mineralocorticoid dose (fludrocortisone) is appropriate.
Could my vivid dreams be a sign of over‑replacement?
Yes. Excess cortisol, especially from a late‑day dose, can trigger intense REM sleep and vivid dreams. Adjusting the timing or slightly lowering the dose often eases the symptoms.
What’s the link between Addison’s disease and sleep apnea?
Weight gain from steroid therapy or fluid retention can increase the risk of airway obstruction during sleep. If you snore loudly or feel unrefreshed after a full night, ask for a sleep study.

Chidi Anslem
October 3, 2025 AT 03:21Living with Addison's disease certainly requires a thoughtful approach to daily routines, and sleep hygiene is a cornerstone of that balance. Aligning medication timing with the body's natural cortisol rhythm not only supports hormonal stability but also fosters a calmer mind before bedtime. Simple habits like a consistent wake‑up time and a dimming‑lights routine can reinforce circadian cues, making the transition to sleep smoother. Hydration matters too-drink enough during the day, but taper off in the evening to prevent nocturnal bathroom trips. If you notice vivid dreams, consider discussing dose adjustments with your endocrinologist; sometimes a smaller evening dose can make a big difference. Light exercise earlier in the day can boost daytime alertness without raising cortisol at night. And remember, the goal is to create a night‑time environment that signals rest, not stress.
Holly Hayes
October 4, 2025 AT 21:01This guide is spot on
Penn Shade
October 6, 2025 AT 23:01When it comes to managing Addison's disease, timing is everything, and the article does a solid job outlining why. First, cortisol follows a diurnal pattern that peaks in the early morning and wanes at night; any deviation can throw off the entire sleep‑wake cycle. Second, taking hydrocortisone early consolidates that natural surge, reducing the risk of nighttime awakenings caused by a sudden cortisol dip. Third, the data from the Endocrine Society in 2023 clearly shows a 30 % increase in sleep latency for doses after 2 p.m., which is a statistically significant figure. Fourth, the recommendation to keep evening doses under 5 mg and before 4 p.m. aligns with pharmacokinetic principles, limiting the drug's half‑life during sleep. Fifth, melatonin can be a useful adjunct, but it should never replace proper steroid scheduling. Sixth, recording your sleep patterns in a journal can help you and your doctor fine‑tune the regimen. Seventh, consistent bedtime routines-like dim lights and a screen‑free window-reinforce melatonin production. Eighth, a light snack with complex carbs before bed can stabilize blood sugar and prevent early‑morning cortisol crashes. Ninth, staying hydrated throughout the day but limiting fluids after dinner reduces bathroom trips that fragment sleep. Tenth, managing stress through mindfulness or gentle yoga can keep cortisol spikes at bay. Eleventh, regular electrolyte checks ensure aldosterone replacement is on point, preventing nocturnal dehydration. Twelfth, if you experience vivid dreams, it often signals a late‑day steroid surge, and adjusting timing can mitigate this. Thirteenth, the table comparing dosing strategies is a quick visual tool that many patients overlook but find extremely helpful. Fourteenth, always discuss any dosage changes with your endocrinologist to avoid under‑ or over‑replacement. Finally, remember that each individual's response can vary, so personalizing these guidelines is essential for optimal rest.
Jennifer Banash
October 8, 2025 AT 11:07It is quite remarkable how the interplay between cortisol and melatonin can dictate the quality of one’s nocturnal repose. While the article provides an exhaustive list of practical measures, one might also consider the impact of ambient temperature-maintaining a bedroom between 60–67 °F is scientifically proven to augment sleep efficiency. Moreover, the suggestion to limit caffeine after noon is not merely anecdotal; caffeine’s half‑life can extend up to 8 hours, thereby potentially elevating cortisol levels well into the evening. The inclusion of a low‑dose melatonin regimen is judicious, yet the reader should be reminded that melatonin is a hormone and, albeit generally safe, should be vetted by a healthcare professional before chronic use. Finally, the emphasis on consistent wake‑up times cannot be overstated: irregularities can blunt the natural cortisol surge, leading to a cascade of nocturnal disturbances.
Stephen Gachie
October 10, 2025 AT 21:27From a philosophical standpoint, the circadian rhythm is a subtle orchestra, and any mistimed glucocorticoid dose is like an off‑beat drum that throws the whole composition into disarray. Your emphasis on aligning medication with the body's innate cortisol peak is spot‑on; the science backs it up, and the practical tips make it accessible. The only nuance I’d add is the role of progressive muscle relaxation before bed, which can further lower sympathetic activity and complement the hormonal strategies you outlined.
Sara Spitzer
October 12, 2025 AT 17:54Great rundown, but I’d point out that the “quick checklist” could benefit from a note about sodium intake for those on fludrocortisone. Adequate salt can prevent those midnight shakiness episodes that many patients forget to mention. Also, a brief mention of the potential for mild sleep‑apnea in weight‑gain scenarios would round out the picture nicely.
Jennifer Pavlik
October 14, 2025 AT 22:41Thanks for the clear guide! If you’re new to managing Addison’s, start with the morning dose tip and build from there. Small changes add up.
Jacob Miller
October 16, 2025 AT 08:01While the article hits many key points, it glosses over the fact that some patients simply cannot shift their dose earlier due to work schedules. In those cases, a split‑dose strategy with a very low evening micro‑dose can be a pragmatic compromise, though it does require close monitoring for nocturnal cortisol spikes.
Anshul Gandhi
October 18, 2025 AT 21:07Don’t be fooled by the “harmless” evening dose claim; pharmaceutical companies often downplay the sleep‑disrupting potential of long‑acting steroids to keep sales high. Independent studies suggest even a 2 mg evening dose can increase insomnia rates by 18 %.
Emily Wang
October 20, 2025 AT 12:01Let’s keep the momentum! Small wins-like turning off screens an hour early-can boost sleep quality dramatically. Celebrate each night you sleep better.
Hayden Kuhtze
October 22, 2025 AT 19:34Oh, brilliant, another article telling us to “avoid evening steroids.” Because the pharmaceutical lobby never pushes for more pills, right? 🙄
Craig Hoffman
October 24, 2025 AT 07:41Quick tip: set a phone alarm for your morning dose so you never miss that 7‑9 am window. It’s easy and saves you from accidental late dosing.
Terry Duke
October 26, 2025 AT 08:41Nice point about dose timing! 😊 Also, remember to check your blood pressure before bed; a quick reading can alert you to nocturnal dips that might be causing those restless nights.
Chester Bennett
October 28, 2025 AT 02:21Well said! Consistency in both medication and bedtime really does set the stage for better rest. Keep it up.
Emma French
October 30, 2025 AT 07:07Appreciate the focus on simple lifestyle tweaks. Small steps are often the most sustainable.
Debra Cine
October 31, 2025 AT 16:27👍 Great advice on the bedtime snack-whole‑grain toast with almond butter is both tasty and stabilizes blood sugar. 🎉
Rajinder Singh
November 3, 2025 AT 02:47Esteemed colleagues, the discourse presented herein admirably consolidates current endocrinological consensus regarding glucocorticoid chronotherapy. Yet, a more exhaustive exploration of pharmacokinetic modeling could further elucidate individualized dosing algorithms.
Samantha Leong
November 4, 2025 AT 23:14I hear you-waking up shaking can be terrifying. Making sure your salt intake is adequate and discussing fludrocortisone dosage with your doctor often eases those episodes.
Taylor Van Wie
November 6, 2025 AT 22:27America’s health guidelines are the only ones that really matter. If you’re not following the US protocols, you’re doing it wrong.
carlee Lee
November 8, 2025 AT 21:41Concise summary: morning dose, consistent bedtime, limit caffeine.