Drug Desensitization Protocol Calculator
What do you do when the only drug that can save your life is the same one that made you break out in hives, swell up, or nearly stop breathing? For many patients, the answer isn’t avoidance-it’s desensitization.
What Is Drug Desensitization, Really?
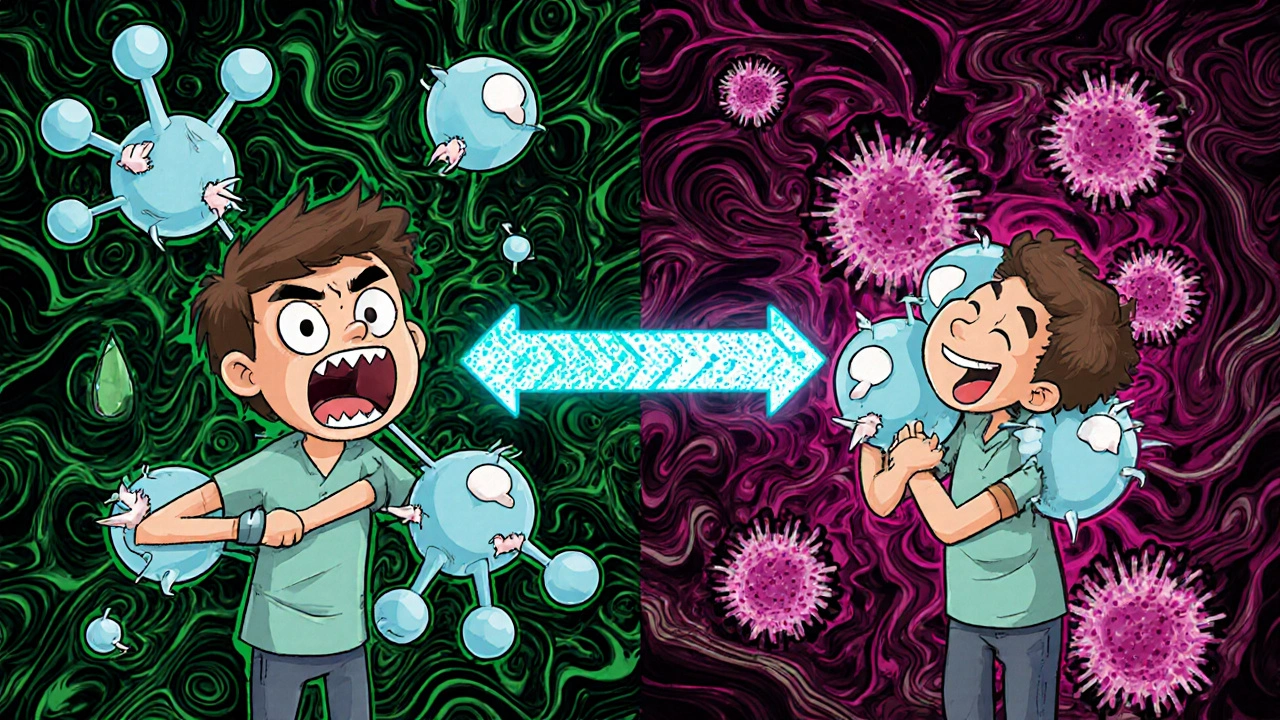
Drug desensitization isn’t about curing an allergy. It’s about temporarily turning off the body’s extreme reaction to a medication so you can take it safely, one tiny dose at a time. This isn’t a trick. It’s a medically supervised process backed by decades of research, mostly developed at Brigham and Women’s Hospital in Boston and now used worldwide.Think of it like slowly walking into a room where the lights are blindingly bright. At first, you squint. Then you blink less. After a few minutes, you can see just fine. That’s what desensitization does to your immune system. It doesn’t erase your allergy. It just gives your body time to adjust-so you can get the treatment you need.
The process works best for immediate, IgE-mediated reactions: hives, swelling, low blood pressure, trouble breathing-all the scary stuff that happens within minutes of taking a drug. It’s less effective for delayed reactions like rashes that show up days later, and it’s absolutely not safe for life-threatening skin conditions like Stevens-Johnson syndrome.
When Is Desensitization the Only Option?
You don’t start desensitization just because you’re nervous. You do it when there’s no other choice.Take antibiotics. If you’re allergic to penicillin, doctors often switch you to something else. But here’s the problem: up to 20% of those alternatives either don’t work as well or cause their own reactions. In cases like osteomyelitis or endocarditis, penicillin is still the gold standard. Desensitization lets you take it-successfully-in 98% of cases, according to studies from Brigham and Women’s Hospital.
Or consider chemotherapy. Drugs like paclitaxel and carboplatin are essential for treating ovarian, lung, and breast cancers. But nearly 1 in 5 patients develop hypersensitivity reactions after just a few doses. Premedication with antihistamines and steroids helps-but still fails in about 10% of cases. Desensitization? Success rates jump to 95-100%. One oncology patient told researchers it was “life-saving.”
Even monoclonal antibodies-used for cancer, autoimmune diseases, and even some infections-are now routinely desensitized when patients react. Before desensitization, many of these patients had to stop treatment entirely. Now, they keep going.
Two Ways to Desensitize: Fast and Slow
There are two main protocols, chosen based on how your body reacts.Rapid Drug Desensitization (RDD) is for immediate reactions. It’s done in a hospital, under constant monitoring. The dose starts at 1/10,000th of the full amount. Every 15 minutes, it doubles. By the end of 4 to 6 hours, you’ve reached the full therapeutic dose. This is the standard for IV antibiotics, chemo drugs, and monoclonal antibodies. Over 400 patients have gone through this at Brigham and Women’s with zero deaths and only mild side effects like flushing or itching in about 8% of cases.
Slow Drug Desensitization (SDD) is for delayed reactions-usually T-cell mediated, like certain rashes or drug-induced liver inflammation. These take longer. You might start with a tiny oral dose and wait 60 to 120 minutes before the next. For aspirin or NSAIDs, it can take two or three days to reach the full dose. There’s no universal rule here. Dosing varies by drug, by patient, and by center. That’s why this should only be done by specialists.
Route matters too. IV is most common for antibiotics (70% of cases). Oral is standard for aspirin and NSAIDs. You can’t just swallow a pill and hope for the best-timing, dilution, and monitoring are everything.
What Happens During the Procedure?
This isn’t something you do at your local pharmacy. Desensitization requires a team: an allergist, nurses trained in anaphylaxis, and a facility with emergency equipment on hand.Before you start, your vital signs are checked: blood pressure, heart rate, oxygen levels. You’re monitored continuously during every dose. If your blood pressure drops or your oxygen levels fall, they stop immediately and treat you like any anaphylactic emergency.
Most people feel fine. Some get mild flushing, itching, or a slight headache. These are common and manageable. Severe reactions happen in fewer than 2% of cases-when protocols are followed correctly.
But here’s the catch: the tolerance doesn’t last. If you stop taking the drug for more than 48 hours, your body forgets. You’ll need to go through the whole process again for the next dose. That’s why it’s used for short-term courses, like a 10-day antibiotic or a set number of chemo infusions.
Why Not Just Avoid the Drug or Use Premedication?
Some doctors try to avoid the drug entirely. But that’s not always safe. For example, if you’re allergic to penicillin and need to treat a resistant infection, the backup drugs may be less effective-or even more toxic.Premedication-giving antihistamines and steroids before the drug-is common. But it’s not reliable. In one study, 4 out of 40 cancer patients still had severe reactions even after premedication. Desensitization cuts that risk dramatically.
And here’s the reality: alternatives often fail because of cross-reactivity. If you’re allergic to penicillin, you might think cephalosporins are safe. But up to 15% of people react to both. Desensitization bypasses that risk entirely.
Who Shouldn’t Try This?
Desensitization isn’t for everyone. It’s a high-risk procedure if misused.It’s absolutely contraindicated for patients who’ve had:
- Stevens-Johnson syndrome
- Toxic epidermal necrolysis
- Severe delayed skin reactions
- History of multi-organ failure from a drug reaction
These are T-cell driven, not IgE-driven. Desensitization won’t help-and could kill you.
It’s also not recommended if you’re not medically stable. If you’re in heart failure, have uncontrolled asthma, or are pregnant with high-risk complications, the stress of the procedure might be too much.
And here’s something many don’t realize: if you’ve had a reaction outside of a hospital, you need to be evaluated by an allergist before even considering desensitization. Not all reactions are true allergies. Some are side effects, like nausea or dizziness, that don’t require desensitization at all.

What Goes Wrong-and How to Avoid It
The biggest problems aren’t the procedure itself. They’re the setup.Studies show 8% of errors happen because the drug isn’t diluted properly. A nurse might misread the concentration. A pharmacy might use the wrong diluent. That’s why standardized kits are now recommended-reducing errors by 75%.
Another 15% of mistakes come from picking the wrong patient. Community hospitals sometimes try this without proper screening. One 2022 study found complication rates were 40% higher in places using generic templates instead of detailed, center-specific protocols.
Training matters. Allergists need to complete 15 to 20 supervised procedures before they’re considered proficient. Nurses need anaphylaxis certification. And the facility? It must have epinephrine, oxygen, IV fluids, and a crash cart ready-right there, in the room.
Patients who’ve been through it say the scariest part isn’t the reaction-it’s the waiting. One Reddit user wrote: “I was terrified every 15 minutes. But when it was over, I cried because I could finally take the medicine that would save my leg.”
The Bigger Picture: Why This Matters Now
Antibiotic resistance is killing 35,000 Americans every year. Many of those deaths could be prevented if we could safely use the best drugs-even in allergic patients.In cancer care, new drugs are coming fast. But nearly a quarter of them carry a risk of hypersensitivity. Desensitization is becoming part of standard oncology protocols-not a last resort.
And the field is evolving. Researchers are now using biomarkers-like basophil activation tests-to predict who will respond before they even start. One 2023 Lancet study showed 89% accuracy. That means less trial and error. Less time in the hospital. Fewer risks.
Future trials are even testing home-based desensitization for stable patients. Imagine being able to take your next chemo dose at home after a successful hospital session. That’s not science fiction-it’s in phase 2 trials with 92% success.
Final Thoughts: It’s Not Magic. But It’s Powerful.
Desensitization isn’t a cure. It’s a bridge. A temporary, medically controlled bridge over a dangerous gap.It doesn’t work for everyone. It’s not easy. It takes time, skill, and resources. But when it’s done right-by the right team, for the right patient-it gives people back their treatment options. Their hope. Their future.
If you’ve been told you can’t take a life-saving drug because of an allergy, ask: has anyone ever tried desensitization? If the answer is no, it’s time to find a specialist.
Can you desensitize to any drug?
No. Desensitization works best for immediate, IgE-mediated reactions to drugs like penicillin, chemotherapy agents, and monoclonal antibodies. It’s not safe for severe delayed reactions like Stevens-Johnson syndrome, toxic epidermal necrolysis, or drug-induced liver failure. The reaction type determines whether it’s even an option.
How long does a desensitization procedure take?
Rapid desensitization for IV drugs usually takes 4 to 6 hours. Slow desensitization for oral drugs like aspirin can take 2 to 3 days, with doses spaced hours apart. The time depends on the drug, the route, and the patient’s reaction history.
Is desensitization permanent?
No. The tolerance is temporary. If you stop taking the drug for more than 48 hours, your immune system “forgets” and you’ll need to repeat the entire process for the next dose. That’s why it’s used for short-term treatments, not lifelong therapy.
Can I do this at my local clinic?
Not safely. Desensitization requires an allergist or immunologist, trained nursing staff, and emergency equipment for anaphylaxis. Most community clinics don’t have the training or resources. Studies show complication rates are 3 times higher when done outside academic medical centers. Always go to a specialized allergy center.
What are the side effects during desensitization?
Mild side effects are common: flushing, itching, headache, or nausea. These usually go away quickly and are managed during the procedure. Severe reactions like low blood pressure or trouble breathing happen in fewer than 2% of cases when protocols are followed correctly. That’s why constant monitoring is required.
Does insurance cover desensitization?
Medicare and most private insurers cover the procedure, but reimbursement often doesn’t cover the full cost. Each session requires 4 to 5 hours of nursing time and 1.5 to 2 hours of physician time. Some smaller hospitals avoid offering it because of financial loss, even when it’s medically necessary.
What’s the success rate?
For immediate hypersensitivity reactions, success rates are 95-100% when performed by experienced teams in proper settings. For penicillin, it’s 98%. For chemotherapy drugs like paclitaxel, it’s over 95%. Failures are rare-and usually tied to improper patient selection or protocol deviations.

Beth Banham
November 4, 2025 AT 11:05This made me cry reading it. I went through desensitization for paclitaxel last year. Thought I was done for. Turns out, my body just needed time to chill out. Now I’m in remission. Thanks for explaining it so clearly.
Brierly Davis
November 6, 2025 AT 09:46YESSSS this is wild how underrated this is 😭 I had a penicillin allergy and needed it for a bone infection-doc said ‘no way’ until we found a specialist. 6 hours of pure terror… then I got to go home and eat tacos like a normal human. Life changing.
Amber O'Sullivan
November 8, 2025 AT 07:52Jim Oliver
November 9, 2025 AT 00:46William Priest
November 9, 2025 AT 02:22lol so you’re telling me you just… slowly give someone a drug they’re allergic to? And it works? Like, what, your body gets used to it? That’s not science, that’s like training a dog to not bark at thunder. Also, why is this not in every hospital? Because money. Always money.
Jennifer Bedrosian
November 9, 2025 AT 10:57OMG I DID THIS. I was so scared. I thought I’d die on the table. But the nurses were so calm and kept telling me ‘you’re safe’ and I just kept thinking ‘if I can get through this, I can get through chemo.’ I cried after it was over. Not from pain-from relief.
Lashonda Rene
November 9, 2025 AT 14:21so i had this friend who was allergic to like every drug ever and she got cancer and they said she couldnt do chemo and she was so sad and then someone told her about this desensitization thing and she did it and now shes fine and she says she feels like she got her life back and i just want everyone to know this is real and it works and you should ask your doctor about it if you think you cant take a medicine because of allergies
Andy Slack
November 10, 2025 AT 03:21This is one of those things that should be common knowledge. We talk about vaccines, we talk about gene therapy, but no one talks about this. Desensitization is quiet magic. It doesn’t make headlines, but it saves lives every day. Hats off to the teams doing this.
Rashmi Mohapatra
November 11, 2025 AT 20:42Abigail Chrisma
November 12, 2025 AT 09:43As someone who’s worked with international patients, I’ve seen this done in India, Brazil, and Kenya-same protocols, same results. It’s not an American invention, it’s a human one. The real issue? Access. Too many people don’t even know this exists. Spread the word.
Ankit Yadav
November 14, 2025 AT 00:29My cousin went through this for carboplatin. Took 3 days. Had to miss work. But now she’s back to teaching kindergarten. The docs said ‘you’ll never do chemo again’-but they didn’t know about slow desensitization. So glad someone wrote this. More people need to hear it.
Meghan Rose
November 14, 2025 AT 17:40Wait, so if you stop taking the drug for more than 48 hours, you have to do it all over again? That’s insane. What if you get sick and miss a dose? Do you just… die? This sounds like a trap. Why not just fix the allergy permanently? Why is this even a thing?
Steve Phillips
November 15, 2025 AT 20:22Oh wow. So we’ve created a $20,000, 6-hour ‘temporary fix’ for a problem we could’ve avoided by… I don’t know… not giving people drugs they’re allergic to? Brilliant. Truly. The healthcare industrial complex strikes again. Also, ‘98% success rate’? That’s just PR. What about the 2% who died? Did they sign a waiver?
Rachel Puno
November 17, 2025 AT 12:55My mom did this for penicillin before her heart surgery. They did it slow-oral doses over two days. She was nervous, but the team made her feel like she was in safe hands. She’s fine now. If you’re scared, ask for the protocol. Ask for the team. You deserve to get the best treatment, not the easiest one.