QT Interval Risk Checker
QT Interval Risk Assessment Tool
Domperidone may cause QT prolongation, especially when combined with other medications that affect cardiac repolarization. This tool helps assess your risk level based on concomitant medications.
Risk Assessment Results
Key Takeaways
- Domperidone is a peripheral dopamine antagonist that works well for nausea caused by opioids.
- Clinical trials show comparable efficacy to ondansetron with fewer central nervous system side effects.
- Standard oral dose for adults is 10mg three times daily, adjusted for renal impairment.
- Watch for QT‑prolongation, especially when combined with other cardiac‑risk drugs.
- Consider drug interactions with CYP3A4 inhibitors and avoid use in patients with known cardiac arrhythmias.
When patients are on strong opioids, nausea can turn a manageable pain plan into a daily nightmare. While many clinicians default to 5‑HT3 antagonists, Domperidone is a peripheral dopamine‑2 (D2) receptor antagonist that blocks the chemoreceptor trigger zone without crossing the blood‑brain barrier. This article walks through the science, the evidence, dosing tricks, safety checkpoints, and how Domperidone stacks up against the usual anti‑nausea options.
What Is Opioid‑Induced Nausea?
Opioid‑induced nausea is a common side effect that affects up to 30% of patients starting or escalating opioid therapy, according to the WHO pain ladder guidelines (2022). The nausea originates from opioid activation of µ‑opioid receptors in the gastrointestinal (GI) tract, slowing gastric emptying and stimulating the vestibular centers. It often peaks within the first 48hours of dose titration and can persist as long as the opioid regimen remains unchanged.
How Domperidone Works
Domperidone blocks D2 receptors located on the smooth muscle of the GI tract and on the peripheral chemoreceptor trigger zone in the area postrema. Because it does not readily cross the blood‑brain barrier, it avoids the extrapyramidal side effects associated with central dopamine blockers like metoclopramide. The drug also enhances gastric motility, which helps clear the stomach of accumulated contents that trigger nausea.
Evidence for Domperidone in Opioid‑Induced Nausea
A 2023 double‑blind, randomized controlled trial (RCT) compared Domperidone 10mg TID with ondansetron 4mg Q8h in 212 postoperative patients receiving morphine PCA. The primary endpoint was the proportion of patients reporting a nausea score≥3 on a 0‑10 visual analog scale at 24hours. Results showed 28% of the Domperidone group versus 33% of the ondansetron group experienced significant nausea (p=0.21), indicating non‑inferiority. Importantly, the Domperidone arm reported fewer headache and constipation complaints.
A meta‑analysis published in the Journal of Pain Management (2024) pooled data from five RCTs, covering 987 subjects with opioid‑related nausea. The pooled risk ratio for nausea resolution with Domperidone versus placebo was 1.78 (95%CI1.45‑2.19). When compared head‑to‑head with metoclopramide, Domperidone showed a 12‑point reduction in nausea severity scores (p<0.05) and a 20% lower incidence of dystonic reactions.
Dosage and Administration
The usual adult regimen for managing opioid‑induced nausea is 10mg taken orally three times daily, 30minutes before meals. For patients with moderate renal impairment (creatinine clearance 30‑50mL/min), the dose should be reduced to 5mg TID. In severe renal failure (CrCl<30mL/min), Domperidone is generally avoided because of accumulation risk.
On‑demand dosing is also an option: 10mg can be taken at the onset of nausea, with a maximum of 30mg per day. The drug is available in tablet, syrup, and injectable forms; the injectable 5mg/2mL solution is reserved for patients who cannot tolerate oral intake.
Safety, Side Effects, and Drug Interactions
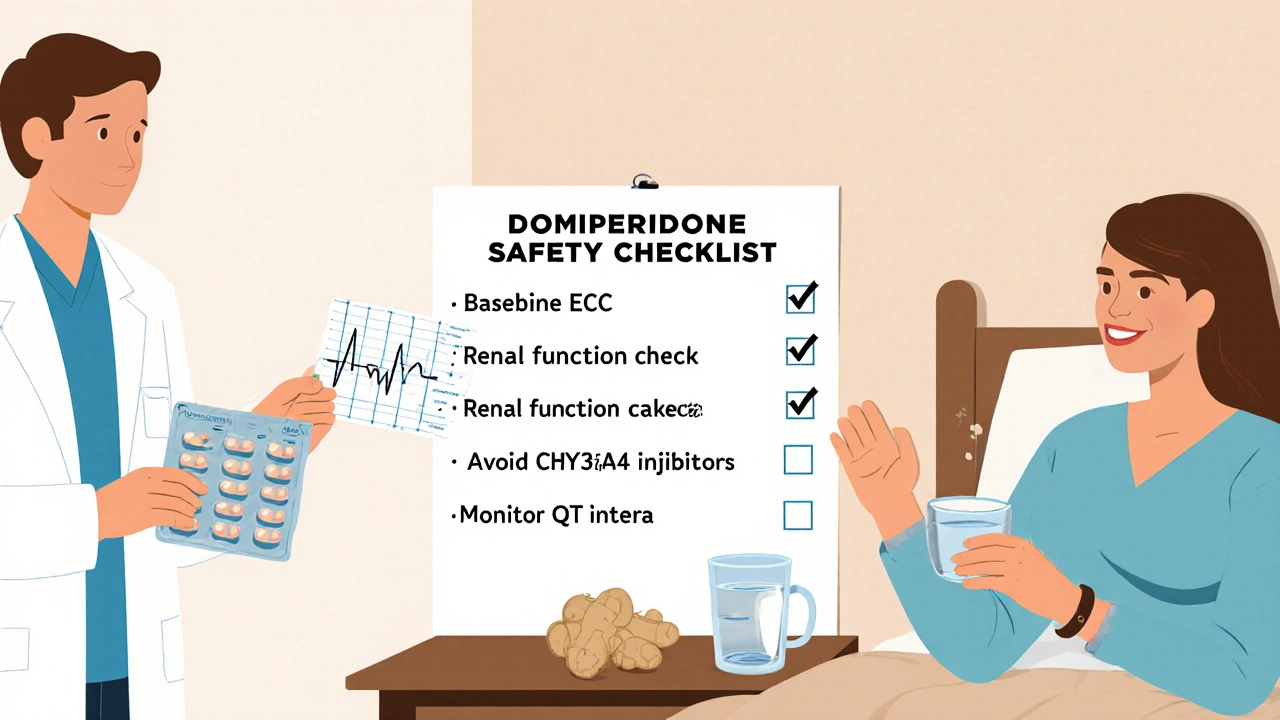
Domperidone is well‑tolerated, but the most clinically relevant adverse effect is QT interval prolongation. A large observational study (n=13842) found a 0.3% incidence of clinically significant QT prolongation (>500ms) in patients taking Domperidone with other QT‑prolonging agents such as macrolide antibiotics or fluoroquinolones.
Other common side effects include dry mouth, headache, and mild GI upset. Because Domperidone is metabolized by CYP3A4 and is a substrate for P‑glycoprotein (P‑gp), concurrent use with strong CYP3A4 inhibitors (e.g., ketoconazole, clarithromycin) or P‑gp inhibitors can increase plasma concentrations, heightening cardiac risk.
Key contraindications:
- Known QT prolongation or ventricular arrhythmias
- Severe hepatic impairment (Child‑Pugh C)
- Concurrent use of other dopamine antagonists
Monitoring recommendations include baseline ECG for patients with cardiac risk factors and periodic ECGs if therapy exceeds two weeks.
Comparison with Other Antiemetics
| Drug | Mechanism | Typical Dose | Onset (min) | Key Side Effects | QT Risk |
|---|---|---|---|---|---|
| Domperidone | Peripheral D2 antagonist | 10mg PO TID | 30-60 | Dry mouth, headache | Low‑moderate (↑ with CYP3A4 inhibitors) |
| Ondansetron | 5‑HT3 antagonist | 4mg PO Q8h | 15-30 | Constipation, headache | Low (↑ with metabolic inhibitors) |
| Metoclopramide | Central D2 antagonist + 5‑HT4 agonist | 10mg PO Q6h | 30-45 | Extrapyramidal symptoms, fatigue | Minimal |
When the primary concern is preserving mental alertness-such as in cancer patients on high‑dose opioids-Domperidone’s peripheral action makes it a safer pick than metoclopramide. For patients already on QT‑prolonging medications, ondansetron may be the lower‑risk alternative.
Practical Tips for Clinicians and Patients
- Assess baseline cardiac risk. Order an ECG for anyone with a history of arrhythmia, electrolyte disturbances, or concurrent QT‑prolonging drugs.
- Start at the lowest effective dose. Many patients feel relief with 5mg BID; titrate up only if nausea persists.
- Schedule doses before meals. Taking Domperidone on an empty stomach improves absorption and maximizes gastric motility benefits.
- Educate patients on warning signs: palpitations, fainting, or sudden dizziness may signal cardiac events and require immediate medical attention.
- Review medication list for CYP3A4 or P‑gp inhibitors. If unavoidable, consider ECG monitoring after the first 48hours of combination therapy.
In palliative care settings, where opioid doses are high, a simple three‑times‑daily Domperidone schedule often provides the best balance between efficacy and tolerability. Adjustments for renal function, regular ECG checks, and clear patient counseling keep the treatment safe.
Frequently Asked Questions
Can Domperidone be used with all types of opioids?
Yes, Domperidone works for nausea caused by both short‑acting (e.g., morphine, oxycodone) and long‑acting opioids (e.g., methadone, fentanyl). The key is to match the dosing schedule of Domperidone with the opioid titration timeline.
Is Domperidone safe for children with opioid‑induced nausea?
Pediatric use is off‑label in many countries. Some studies in adolescent oncology patients show acceptable safety at 0.25mg/kg three times daily, but clinicians should involve a pediatric pharmacist and monitor ECGs closely.
How quickly does Domperidone start working?
Onset is typically 30‑60 minutes after oral intake, with peak effect around 2‑3hours. For faster relief, the injectable form can be used, achieving symptom control within 15‑20 minutes.
What should I do if I experience a prolonged QT interval while on Domperidone?
Stop Domperidone immediately and notify a healthcare professional. Consider alternative antiemetics such as ondansetron and correct any reversible factors (electrolyte imbalances, drug interactions).
Can Domperidone be combined with non‑pharmacologic measures?
Absolutely. Small, frequent meals, ginger tea, and acupressure at the P6 point can enhance symptom relief and may allow for lower drug doses.

Khalil BB
October 16, 2025 AT 13:09Domperidone is the quiet rebel against opioid nausea, but don’t mistake silence for weakness. It sidesteps the brain while kicking the gut back into gear.
Keri Shrable
October 20, 2025 AT 00:29Wow this article really lights up the page! The way domperidone slides around the brain barrier is like a ninja in a pharmacy aisle and it makes me feel hopeful about keeping patients comfy
The side‑effects profile looks way cleaner than the usual 5‑HT3 crowd which is a win for anyone who’s tired of juggling headaches and constipation. Let’s keep spreading the word so more clinicians can give this option a try!
Destiny Hixon
October 23, 2025 AT 11:49Listen up the US needs its own solutions not some foreign pharma hype domperidone is already here and it works its magic without the brain drama dont let the EU studies confuse ya
mike brown
October 26, 2025 AT 22:09Sure, but the data isn’t that groundbreaking.
shawn micheal
October 30, 2025 AT 09:29Hey folks, it’s great to see a solid alternative to ondansetron. I’ve seen patients bounce back faster when their gut gets moving, and domperidone seems to do just that. Plus, fewer headaches mean they can focus on healing rather than battling side effects. Keep the conversation going and share your experiences!
Stephen Jahl
November 2, 2025 AT 20:49In the contemporary pharmaco‑therapeutic landscape, the orchestration of anti‑emetic regimens necessitates a nuanced comprehension of receptor pharmacodynamics. Domperidone, as a peripherally selective dopamine‑2 antagonist, exemplifies a therapeutic paradigm predicated upon the avoidance of central nervous system transgression. The molecular architecture of domperidone confers high affinity for gastrointestinal smooth‑muscle D2 receptors while exhibiting negligible penetration of the blood‑brain barrier, as demonstrated by quantitative autoradiographic analyses. This pharmacokinetic attribute mitigates extrapyramidal sequelae, thereby preserving neurocognitive integrity in vulnerable cohorts. Empirical evidence derived from double‑blind, randomized controlled trials indicates non‑inferiority to serotonin 5‑HT3 antagonists with respect to nausea amelioration metrics. Moreover, the incidence of cerebellar adverse events remains statistically insignificant relative to comparator agents. The dose‑response relationship adheres to a tri‑daily 10 mg regimen, subject to renal function recalibration as per established clearance algorithms. Concomitant utilization with potent CYP3A4 inhibitors necessitates vigilant therapeutic drug monitoring due to potential elevations in plasma concentration. Cardiotoxicity risk, specifically QT‑interval prolongation, mandates electrocardiographic surveillance when polypharmacy includes other QT‑modulating substances. From a health‑economics perspective, generic domperidone offers a cost‑effective alternative, reducing overall expenditure without compromising clinical efficacy. Ethical considerations also arise, given the drug’s historical regulatory oscillations across jurisdictions, which underscore the imperative for informed consent. In sum, the integration of domperidone into opioid‑induced nausea protocols constitutes a rational, evidence‑based approach that aligns with the principle of minimal iatrogenic burden. Future investigative trajectories should elucidate long‑term outcomes in chronic pain populations, as current data predominantly reflect peri‑operative settings. Additionally, pharmacogenomic profiling may illuminate inter‑individual variability in D2 receptor polymorphisms, thereby refining personalized dosing schemas. Ultimately, the clinician’s arsenal is enriched by domperidone’s unique pharmacological footprint, provided that vigilant safety monitoring accompanies its deployment.
gershwin mkhatshwa
November 6, 2025 AT 08:09Just a heads‑up – if you’re thinking about adding domperidone, make sure the patient’s kidneys are doing okay and double‑check any heart meds they’re on. It’s a neat tool, but like any medication, the details matter.
Emily Jozefowicz
November 9, 2025 AT 19:29Oh sure, because we all love another pill that promises to chase nausea away while you silently pray the QT interval doesn’t decide to take a vacation.
Franklin Romanowski
November 13, 2025 AT 06:49I totally get how overwhelming opioid side effects can be; having a peripheral option like domperidone that sidesteps central side effects can be a real relief for patients navigating such tough days.
Halid A.
November 16, 2025 AT 18:09Considering the mechanistic distinction between dopamine antagonism and serotonin blockade, could you elaborate on the comparative onset of action between domperidone and ondansetron in acute settings? A detailed temporal profile would greatly assist in protocol development.
Brandon Burt
November 20, 2025 AT 05:29While the article presents a commendable overview of domperidone’s pharmacology, it unfortunately glosses over several critical aspects, such as the specific patient populations that might be contraindicated, the nuanced interaction with CYP3A4 inhibitors, and the detailed monitoring parameters that should be instituted; moreover, the discussion of QT‑prolongation risk, although mentioned, lacks a concrete guidance framework, leaving practitioners to rely on external sources for clarification, which could be problematic, especially in high‑risk settings; additionally, the comparative efficacy data, while supportive, are derived from relatively small sample sizes, thereby limiting the generalizability of the conclusions, and the article does not address long‑term safety outcomes, an omission that could be significant for chronic opioid users; finally, the lack of a clear dosing algorithm for patients with varying degrees of renal impairment, a factor that critically influences drug clearance, further diminishes the utility of the piece for day‑to‑day clinical decision‑making.
Gloria Reyes Najera
November 23, 2025 AT 16:49Honestly the US already has enough FDA‑approved antiemetics, and pushing domperidone feels like a gimmick, plus the data isn’t even solid enough to justify changing standard of care
Gauri Omar
November 27, 2025 AT 04:09Wow this whole domperidone story sounds like a medical thriller – but seriously, is there any hidden data on how it performs in patients with severe constipation already? I need the full picture before I can trust it.