When your kidneys start to fail, your body doesn’t just slow down-it starts to swell. Edema in chronic kidney disease (CKD) isn’t just a nuisance. It’s a sign your body is drowning in fluid it can’t get rid of. You might notice your ankles puffing up, your shoes feeling tighter, or your face looking puffy in the morning. If you’re living with stage 3 or worse CKD, this isn’t rare. It’s common. And it’s dangerous if left unchecked.
Why Your Kidneys Cause Swelling
Your kidneys are like filters. They pull out extra water and salt from your blood and send it out as urine. But when they’re damaged-say, from diabetes, high blood pressure, or long-term inflammation-they lose their ability to do this well. Sodium builds up. Water follows sodium. And suddenly, fluid leaks out of your blood vessels and into your tissues. That’s edema. This doesn’t happen overnight. In early CKD (stages 1-2), your kidneys still manage. But by stage 3, when your eGFR drops below 60, things start slipping. By stage 4 or 5, fluid overload becomes a daily battle. The swelling usually shows up first in your legs and feet, then around your eyes, and in advanced cases, even in your belly (ascites).Diuretics: The Go-To Drug, But With Risks
Doctors reach for diuretics first because they work fast. These are the pills that make you pee more. But not all diuretics are the same, and not all are safe for every stage of CKD. For people with eGFR under 30, loop diuretics like furosemide (Lasix), bumetanide, or torsemide are the standard. They work on the part of the kidney that handles the most sodium. A typical starting dose is 40-80 mg daily. If that doesn’t help, doctors may bump it up by 20-40 mg every few days. Some patients end up on 160-320 mg a day. But here’s the catch: the stronger the diuretic, the more it can hurt your kidneys. A 2016 NIH study found that people on high-dose diuretics lost kidney function three times faster than those who weren’t. Their eGFR dropped an average of 3.2 mL/min/year, compared to 1.7 for non-users. And the risk of needing dialysis jumped by 47% in just 12 months. For people with better kidney function (eGFR over 30), thiazides like hydrochlorothiazide can help. But when kidney function is low, they barely work. That’s why doctors sometimes combine a loop diuretic with a thiazide-called sequential nephron blockade. It boosts fluid removal by 20-30%, but it also raises the risk of sudden kidney injury by 23%. And then there’s spironolactone. It’s a potassium-sparing diuretic, often used if you also have heart failure. But in late-stage CKD, it can spike your potassium to dangerous levels. Over 25% of patients with stage 4 or 5 CKD develop hyperkalemia on this drug. That’s why blood tests are non-negotiable.Salt Restriction: The Most Underused Tool
If you’re taking diuretics but still swelling, you’re probably still eating too much salt. Not the salt shaker. The hidden stuff. Processed food is the real villain. Bread, canned soup, deli meats, frozen meals-they’re loaded. Two slices of bread? That’s 300-400 mg of sodium. One cup of canned soup? 800-1,200 mg. Two ounces of deli turkey? 500-700 mg. Add that up over a day, and you’re easily over 3,000 mg-even if you never touch the salt shaker. The National Kidney Foundation says you should aim for no more than 2,000 mg of sodium a day. For advanced CKD, they recommend 1,500 mg. That’s not easy. But it works. Studies show that strict salt restriction can cut edema by 30-40% in early CKD-without any pills. It’s not just about salt. It’s about all fluids. Soups, yogurt, fruits like watermelon, even ice cream count. In late-stage CKD, doctors often limit total fluid intake to 1,500-2,000 mL per day. That’s about 6-8 cups. And yes, that includes the water you drink with your meds. Most patients struggle with this. In a 2024 survey of over 1,200 people with CKD, 72% said they couldn’t give up salty tastes. 65% said eating out or with family was too hard. That’s why dietitians are critical. Three to four sessions with a renal dietitian can make the difference between control and crisis.
Compression Therapy: When Pills and Diet Aren’t Enough
If your legs are swollen, walking around in compression stockings isn’t just a suggestion-it’s part of the treatment plan. Graduated compression stockings (30-40 mmHg at the ankle) squeeze your legs just enough to push fluid back toward your heart. A 2022 study showed they reduce leg volume by 15-20% after four weeks. That’s measurable. That’s real. But here’s the problem: most people stop wearing them. A 2022 University of Michigan study found only 38% kept using them past three months. Why? They’re hard to put on. They itch. They feel tight. Some people just hate how they look. The fix? Combine compression with movement. Walking 30 minutes five days a week improves lymphatic drainage and cuts edema by 22% compared to sitting still. Elevating your legs above your heart for 15-20 minutes a few times a day helps too. It’s simple, but it works. For severe cases-especially with nephrotic syndrome or massive swelling-intermittent pneumatic compression devices can help. These machines inflate and deflate around your legs in cycles, mimicking muscle movement. One 2020 study found they reduced leg circumference 35% more than regular stockings alone.The Big Picture: Balance Over Aggression
There’s a dangerous myth: the more you pee, the better. But in advanced CKD, that’s not true. Pushing too hard with diuretics can crash your blood pressure, cause kidney injury, or trigger dangerous electrolyte shifts. Dr. David Wheeler, a lead author of the KDIGO guidelines, says: “The therapeutic window for diuretics in advanced CKD is narrow.” Too little fluid? You get dizzy, weak, maybe even faint. Too much? You’re at risk for heart failure, lung congestion, or death. The goal isn’t to make you “dry.” It’s to get you to your dry weight-the weight where you feel your best, with no swelling, no shortness of breath, and no fatigue. That’s usually a loss of 0.5 to 1.0 kg per day in acute cases. And it’s not about speed. It’s about sustainability. The best outcomes come from a team approach: a nephrologist, a renal dietitian, and a physical therapist working together. In the Mayo Clinic’s patient registry, 75% of stage 3-4 CKD patients achieved good edema control in eight weeks with multidisciplinary care. Only 45% did with standard care.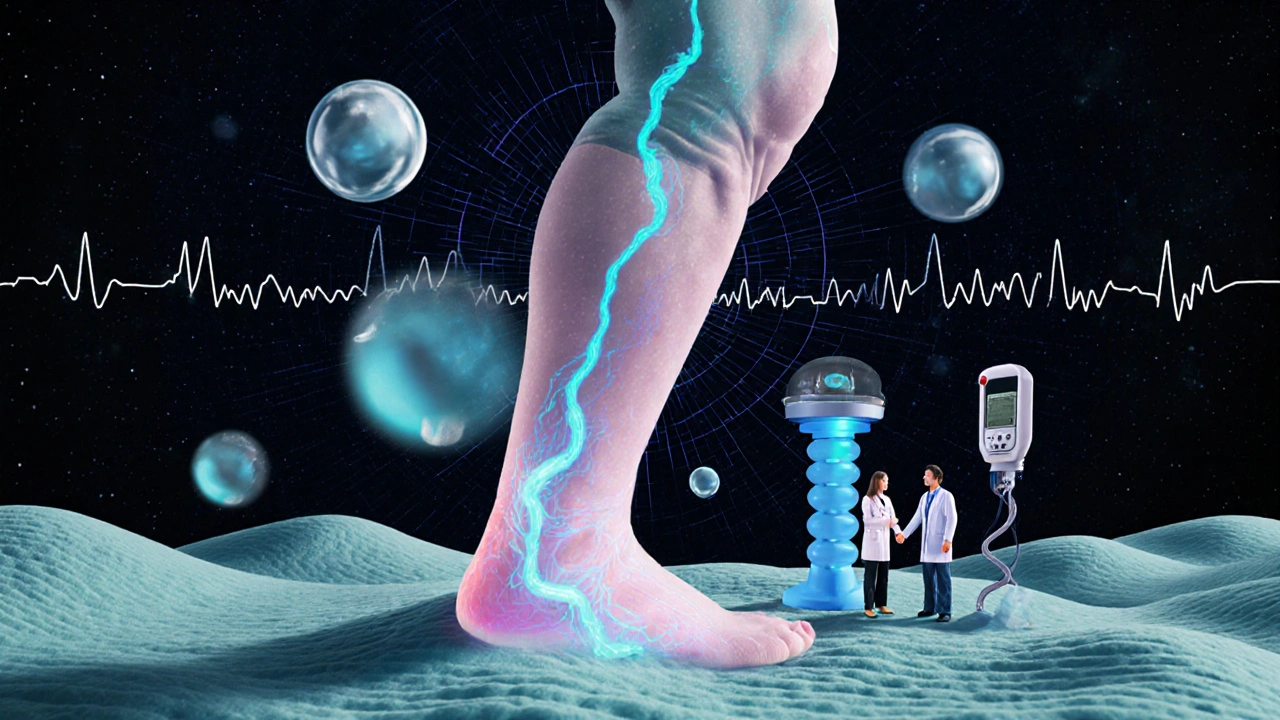
What’s Coming Next
New tools are on the horizon. In March 2025, the FDA approved an injectable form of furosemide specifically for advanced CKD. For patients with eGFR under 15, it clears fluid 38% faster than oral pills. That’s huge for those who can’t absorb meds through the gut. Another promising area is bioimpedance spectroscopy (BIS). This machine measures body water without a needle. It’s not in every clinic yet, but in the NIH’s FOCUS trial, using BIS to guide diuretic dosing cut hospitalizations for fluid overload by 32%. Vaptans-drugs that block water retention-were once thought to be the future. But a 2024 trial was stopped because of liver damage. So for now, the old tools-salt control, smart diuretics, and compression-are still the backbone.Real Talk: What Works in Real Life
Let’s be honest. Managing edema in CKD is hard. It’s not just about taking pills. It’s about changing how you eat, how you move, how you think about your body. One patient I spoke with-let’s call her Maria-had stage 4 CKD and swollen legs for over a year. She was on furosemide, but still bloated. Her doctor told her to cut salt. She laughed. “I don’t even use salt,” she said. Then she realized: her favorite canned chili, her lunchtime turkey sandwich, her soy sauce on rice-those were the culprits. She started reading labels. She switched to no-salt-added beans. She made her own soup. Within three weeks, her ankles were less puffy. She started walking daily. She bought compression socks. She didn’t love them-but she wore them. In two months, her weight stabilized. Her doctor said she’d avoided a hospital trip. It’s not glamorous. It’s not a miracle drug. But it works.When to Call Your Doctor
Swelling isn’t always just edema. If you notice:- Sudden weight gain of more than 2 kg (4.4 lbs) in 2 days
- Shortness of breath, especially when lying down
- Chest pain or rapid heartbeat
- Confusion, dizziness, or fainting
- Red, warm, swollen leg (could be a clot)
Can I stop taking diuretics if I eat less salt?
Maybe, but don’t stop without talking to your doctor. Salt restriction can reduce swelling significantly, especially in early CKD. But if you’ve been on diuretics for a while, your body may have adapted. Stopping suddenly can cause fluid to rebound. Your doctor will likely lower your dose slowly while monitoring your weight and blood pressure.
Why do I need compression socks if I’m already on diuretics?
Diuretics remove fluid from your bloodstream, but they don’t fix the pressure in your leg veins. Compression socks help push that pooled fluid back up toward your heart. Think of it like this: diuretics drain the bathtub, but compression socks stop the water from pooling in the corners. They work together.
Is it safe to use over-the-counter diuretics for CKD swelling?
No. Over-the-counter diuretics (like herbal pills or “water pills” sold online) are not regulated and can be dangerous. They may contain unapproved ingredients, cause dangerous drops in blood pressure, or worsen kidney function. Always use only medications prescribed by your nephrologist.
How long does it take to see results from salt restriction?
Most people notice less swelling in 2-4 weeks with strict sodium control. Some feel better in just a few days. The key is consistency. One high-sodium meal can undo days of progress. Tracking your intake with a food app can help you stay on track.
Can compression therapy make swelling worse?
Only if used incorrectly. Compression that’s too tight, worn too long, or applied over open sores or infections can cause harm. Always get fitted by a professional. If your skin turns purple, numb, or painful, stop using them and call your doctor.
What’s the best way to track fluid buildup at home?
Weigh yourself every morning, right after using the bathroom and before eating or drinking. Write it down. A sudden gain of 1-2 kg (2-4 lbs) in 24-48 hours is a red flag. Also, check your ankles. Press your finger into the skin near your ankle bone. If it leaves a dent that takes a few seconds to bounce back, that’s pitting edema-and it’s time to call your care team.
If you’re managing edema in CKD, you’re not alone. It’s a daily grind-but small, consistent steps make a big difference. Focus on what you can control: your salt, your movement, your weight, and your communication with your care team. The goal isn’t perfection. It’s progress.
Pravin Manani
November 21, 2025 AT 10:51Loop diuretics in eGFR <30 are indeed first-line, but the nephron blockade strategy with thiazides is underutilized in community practice. The 20-30% additive diuresis is clinically meaningful, especially when combined with sodium restriction. The real challenge is adherence to fluid limits-most patients don’t realize that yogurt and soup count. Renal dietitians should be mandatory referrals, not optional.
Corra Hathaway
November 21, 2025 AT 11:11Compression socks are the unsung heroes of CKD management 😅 I wore them for 3 weeks and my ankles stopped looking like inflated balloons. Also, walking 30 min/day is free therapy. Who knew? 🙌
Clifford Temple
November 22, 2025 AT 21:13Why are we letting Big Pharma push these expensive injectables when salt restriction and compression have been proven for decades? This is just another money grab. America’s healthcare system is broken.
Simone Wood
November 23, 2025 AT 21:09Did you know that in the UK, some NHS trusts now offer free compression garments to CKD patients? Here in the States, you’re lucky if your insurance covers one pair. This is why I can’t trust the system. My cousin had to sell her car to afford her meds. 😭
Shawn Sakura
November 24, 2025 AT 11:47Just wanted to say-this post saved my life. I had stage 4 CKD and was in and out of the hospital every month. Started reading labels, cut out canned soup, started walking, wore my socks. Lost 8 lbs in 3 weeks. No more pitting edema. Thank you.
Swati Jain
November 26, 2025 AT 06:25Let’s be real-no one actually eats 1500mg of sodium a day unless they’re living on boiled broccoli and water. Even ‘low-sodium’ soy sauce has 600mg per tablespoon. This whole ‘salt restriction’ thing is a myth perpetuated by nephrologists who’ve never eaten real food.
jim cerqua
November 27, 2025 AT 16:17DIURETICS ARE KILLING PEOPLE. I’ve seen it. My uncle was on 320mg of Lasix daily. His kidneys crashed. He went on dialysis in 6 months. This isn’t medicine-it’s a slow, bureaucratic murder. And now they’re pushing INJECTABLES? What’s next? IV salt restriction?
Nikhil Purohit
November 29, 2025 AT 03:10Swati, you’re missing the point. It’s not about eating boiled broccoli-it’s about swapping out the hidden sodium bombs. My mom switched from canned chili to homemade beans with cumin and lime. She didn’t feel deprived. She felt in control. Small swaps, big results.
Paula Jane Butterfield
November 30, 2025 AT 16:23As an Indian-American with CKD, I get how hard it is to give up masala chips and pickles. But I started using lemon juice and black salt (kala namak) instead of regular salt. My family thought I was crazy… until they noticed I wasn’t puffy anymore. Cultural food doesn’t have to be high sodium. It’s about adaptation, not elimination.
Florian Moser
December 1, 2025 AT 03:01Compression therapy isn’t optional-it’s foundational. The fact that only 38% of patients stick with it speaks to a failure in patient education, not patient laziness. We need better fitting tools, more education, and maybe even compression sock fashion lines. Seriously-why can’t they come in patterns?
Leo Tamisch
December 2, 2025 AT 10:42Wow. So much science. So many numbers. So little soul. I mean, have you ever just… sat with your feet up and listened to your body? Diuretics are just a bandaid on a broken system. Maybe the real solution is meditation, grounding, and eating organic kale. 🌿✨
Chris Vere
December 3, 2025 AT 19:15The data here is compelling but incomplete. What about the role of inflammation in fluid retention? The paper doesn’t address cytokine-driven sodium retention, which is increasingly recognized in CKD. Also, the mention of BIS is promising but not scalable. We need low-cost alternatives for low-resource settings. This feels like a conversation happening in elite clinics while patients in Lagos or Mumbai are still guessing.
Donald Frantz
December 5, 2025 AT 03:12Has anyone considered that diuretic resistance isn’t always due to poor compliance? What about altered renal tubular transport in advanced CKD? The pharmacokinetics change. Maybe we need more research on transporter expression profiles rather than just upping doses. This is basic nephrology.
Julia Strothers
December 6, 2025 AT 01:00Wait-so you’re telling me the FDA approved an injectable diuretic… right after the pharmaceutical lobby donated $12 million to the nephrology association? Coincidence? I think not. This is how they keep people dependent. They don’t want you to heal. They want you to keep buying.
Erika Sta. Maria
December 6, 2025 AT 10:15Actually, the real problem is that diuretics are overprescribed because doctors are lazy. Why not just do dialysis earlier? Or better yet-why not fix the kidneys? We’ve been stuck in this 1980s model of managing symptoms instead of curing disease. The real innovation isn’t in pills or socks-it’s in regenerative medicine. But nobody wants to fund that.