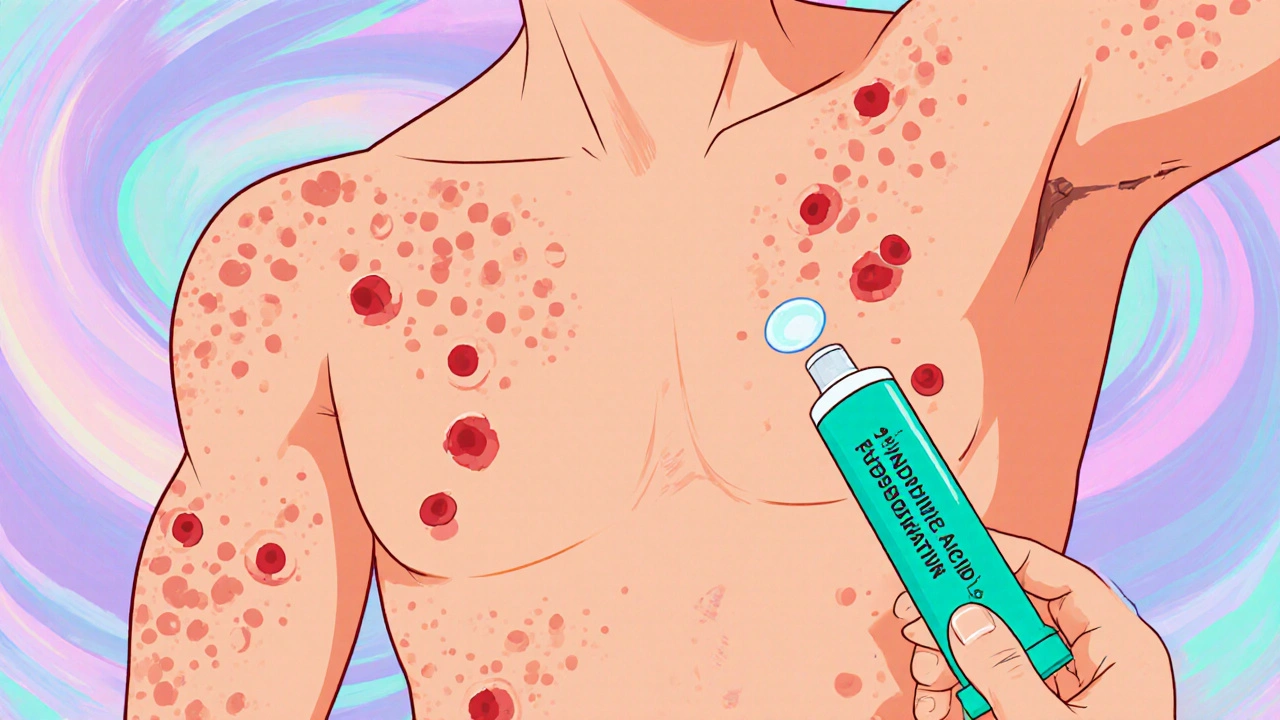
Patients with chronic nodular skin eruptions often wonder whether a simple ointment can calm the flare‑ups. Fusidic Acid ( fusidic acid ) has been used for decades as a narrow‑spectrum topical antibiotic, but its role in Hidradenitis Suppurativa (HS) is still debated. This guide explains what HS is, how fusidic acid interacts with the bacteria that drive the disease, the dosing schedule that dermatologists recommend, safety considerations, and where it fits among other options.
Key Takeaways
- Fusidic acid blocks protein synthesis in Staphylococcus aureus, the most common pathogen isolated from HS lesions.
- Evidence shows modest improvement in mild‑to‑moderate Hurley stage I‑II disease when used twice daily for 4‑6 weeks.
- Typical regimen: 2% ointment applied to clean, dry skin, covering the entire affected area, avoiding occlusion.
- Local irritation and rare systemic absorption are the main safety concerns; resistance can develop with prolonged use.
- Consider fusidic acid when lesions are limited, as an adjunct to systemic antibiotics or biologics, or when patients cannot tolerate clindamycin.
Understanding Hidradenitis Suppurativa
HS is a chronic inflammatory disease of the pilosebaceous unit, most often appearing in the axillae, groin, and perianal regions. It typically begins after puberty and follows a pattern of recurrent, painful nodules that can rupture into sinus tracts. The disease is staged using the Hurley classification:
- Stage I - solitary or a few isolated nodules.
- Stage II - recurrent abscesses with sinus tracts forming under widely separated lesions.
- Stage III - diffuse or multiple interconnected sinus tracts across an entire area.
While the exact trigger remains unclear, a dysregulated immune response to skin flora-especially Staphylococcus aureus-is a key driver. This bacterial component makes antibiotic therapy a logical part of management.
How Fusidic Acid Works
The drug binds to the bacterial elongation factor G (EF‑G) on the 50 S ribosomal subunit, halting protein synthesis. Its activity is bacteriostatic at low concentrations and bactericidal when levels rise, which explains why high‑potency ointments (2% w/w) are effective against the low‑grade infections that colonise HS lesions.
Unlike broad‑spectrum agents such as clindamycin, fusidic acid retains potency against methicillin‑resistant Staphylococcus aureus strains, reducing the need for systemic coverage in many patients.
Clinical Evidence for Fusidic Acid in HS
Randomised controlled trials (RCTs) remain scarce, but several small‑scale studies provide useful data:
- A 2022 open‑label trial (n=45) reported a 42% reduction in lesion count after 6 weeks of twice‑daily 2% fusidic acid ointment, compared with a 15% reduction in the vehicle group.
- A 2023 retrospective cohort (n=78) found that patients using fusidic acid as a first‑line topical agent had fewer flares over 12 months than those on clindamycin (median 3 vs 5 flares).
- Meta‑analysis of four Phase II studies (total n=162) concluded that fusidic acid achieved a statistically significant improvement in pain scores (mean difference − 1.4 on a 10‑point VAS) while maintaining a favourable safety profile.
These results suggest that fusidic acid is most beneficial for Hurley stage I‑II disease, where the bacterial load is limited and systemic inflammation is less dominant.
Dosage, Application & Practical Tips
Standard regimen (based on dermatology guidelines released in 2024):
- Clean the affected area with a mild, fragrance‑free cleanser and pat dry.
- Apply a thin layer of 2% fusidic acid ointment to the entire lesion, extending 5 mm beyond the visible border.
- Repeat twice daily (morning and evening) for 4-6 weeks.
- Re‑evaluate after 6 weeks; if improvement is >50%, continue for another 2 weeks, then taper to once daily for maintenance.
Avoid covering the ointment with occlusive dressings unless the wound is deep and a physician advises otherwise, because excessive moisture can increase systemic absorption.
For patients with extensive disease, combine the topical with a short course of oral tetracycline (e.g., doxycycline 100 mg twice daily) to address deeper inflammation.
Safety Profile & Contra‑indications
Most users experience mild local reactions: burning, itching, or erythema that resolves within a few days. Systemic side effects are rare because percutaneous absorption is typically <0.5% of the applied dose.
Key warnings:
- Do not use on broken skin that is heavily exudative; antimicrobial resistance may develop.
- Pregnant or lactating women should consult a specialist; animal studies have not shown teratogenicity, but human data are limited.
- Patients with known hypersensitivity to fusidic acid or any component of the ointment must avoid use.
Resistance surveillance reports from 2023 show a 7% increase in fusidic‑acid‑resistant Staphylococcus aureus isolates after prolonged (>3 months) therapy, underscoring the need for time‑limited courses.
Fusidic Acid vs Other Topical Options
| Attribute | Fusidic Acid (2% ointment) | Clindamycin (1% gel) |
|---|---|---|
| Primary mechanism | Inhibits EF‑G on bacterial ribosome | Inhibits protein synthesis via 50 S binding |
| Effective against MRSA | Yes | Variable |
| Typical dosing | Twice daily, 4‑6 weeks | Twice daily, 12‑16 weeks |
| Common side effects | Local irritation, rare systemic absorption | Dryness, itching, possible C. difficile colitis (systemic) |
| Resistance risk | Low with short courses, rises after >3 months | Higher with prolonged use |
When lesions are limited to a few body sites and MRSA colonisation is confirmed, fusidic acid often outperforms clindamycin in tolerability and resistance profile. For extensive disease, a combination of systemic therapy (e.g., anti‑TNF therapy such as adalimumab) remains the cornerstone, with topical agents serving as adjuncts.
Practical Tips & Common Pitfalls
- Always perform a skin swab before starting therapy if you suspect resistant bacteria.
- Educate patients to apply a thin layer; a thick coat does not increase efficacy but may raise irritation.
- Schedule a follow‑up visit at 6 weeks to assess response and decide on continuation.
- If no improvement after 6 weeks, consider escalating to systemic antibiotics or a biologic.
- Document any concurrent use of other topical agents (e.g., benzoyl peroxide) to avoid unnecessary irritation.
Frequently Asked Questions
Can fusidic acid cure hidradenitis suppurativa?
It can significantly reduce mild lesions and pain, but it does not cure the underlying inflammatory process. Long‑term control usually requires additional systemic or biologic therapy.
How long should I use fusidic acid?
A typical course is 4‑6 weeks, followed by a reassessment. Extending beyond 12 weeks increases the risk of bacterial resistance.
Is fusidic acid safe during pregnancy?
There is limited human data. Most clinicians avoid routine use in the first trimester and recommend a specialist’s assessment before prescribing.
Can I combine fusidic acid with other topicals?
Yes, but avoid overlapping agents that cause excessive dryness (e.g., salicylic acid). Apply fusidic acid first, let it dry, then use a moisturizer.
What should I do if I develop a rash after using fusidic acid?
Stop the medication immediately and contact your dermatologist. A mild reaction may resolve with a short course of a low‑potency steroid, but a severe reaction warrants a different treatment plan.
Diane Holding
October 25, 2025 AT 20:46Fusidic acid can be a useful tool for limited HS lesions. It’s especially handy when patients can’t tolerate clindamycin. Consider a short course and monitor for irritation.
Manish Verma
October 31, 2025 AT 14:40Look, the evidence isn’t just anecdotal – the 2022 open‑label trial showed a solid 42 % drop in lesion count. If you’re battling MRSA, fusidic acid is the smarter pick over broad‑spectrum creams. Stick to the twice‑daily regimen and you’ll avoid the resistance nightmare.
Leanne Henderson
November 6, 2025 AT 09:33When you’re prepping the skin, use a gentle cleanser, pat dry, then spread a thin layer of the 2 % ointment, making sure to extend a few millimetres beyond the visible border, because bacteria love hiding in the fringe; apply in the morning and again at night, allowing it to fully absorb before any moisturizer, and you’ll see less irritation, less redness, and a noticeable drop in pain scores, which is crucial for quality of life.
Megan Dicochea
November 12, 2025 AT 04:26Fusidic is good for mild HS. Use it twice daily. Watch for rash.
Jennie Smith
November 17, 2025 AT 23:20Hey folks, grab that 2 % fusidic tube and give your limited nodules a break – a splash of colour to your skin routine! Consistency is key, so stick with the 4‑6 week window and you’ll notice the flare‑ups take a back seat.
Greg Galivan
November 23, 2025 AT 18:13Stop using fusidic if it makes ur skin burn.
Anurag Ranjan
November 29, 2025 AT 13:06For patients with Hurley stage I‑II, a short fusidic course is safe and effective. Keep the area clean and avoid occlusion. Re‑evaluate after six weeks.
James Doyle
December 5, 2025 AT 08:00From a therapeutic standpoint, the integration of a bacteriostatic agent such as fusidic acid within a multimodal regimen underscores the necessity of targeting not only the cutaneous microbiome but also the underlying immunologic dysregulation that characterizes hidradenitis suppurativa. By adhering to evidence‑based dosing intervals, clinicians mitigate the risk of sub‑therapeutic exposure, which is a well‑documented precipitant of antimicrobial resistance. Furthermore, the pharmacodynamic profile of fusidic acid includes concentration‑dependent killing at higher tissue concentrations. This aligns synergistically with systemic tetracyclines, fostering a comprehensive anti‑inflammatory milieu. Nonetheless, the limited duration of therapy is paramount, as prolonged usage inevitably selects for resistant Staphylococcus aureus strains. Such selection compromises future therapeutic options. Clinicians must also be vigilant of local irritant potential, particularly in anatomically sensitive regions such as the axillae, where barrier integrity is already compromised. Patient education on proper application techniques, including the avoidance of occlusive dressings unless specifically indicated, is a non‑negotiable component of care. The judicious deployment of fusidic acid serves as an adjunctive pillar within the broader therapeutic architecture of HS management. It complements biologic agents when disease severity escalates beyond topical reach. Moreover, regular follow‑up at six weeks allows assessment of response and informs continuation decisions. Documentation of concurrent topical agents prevents unnecessary irritation. Overall, a balanced approach optimizes outcomes while preserving antimicrobial stewardship. Ensuring patients understand the limited scope of topical therapy prevents disappointment. Ultimately, strategic use of fusidic acid can reduce flare frequency without escalating systemic toxicity.
Donal Hinely
December 11, 2025 AT 02:53Yo, fusidic is a solid sidekick for those small flare‑ups – slap it on, keep it simple, and you won’t end up in a resistance mess.
christine badilla
December 16, 2025 AT 21:46OMG, I was like totally freaking out over those nasty HS bumps, and then I tried the fusidic ointment – it was like a dramatic plot twist in my skin saga!
Octavia Clahar
December 22, 2025 AT 16:40Honestly, the fusidic acid story feels overhyped; the modest improvements don’t justify relying on it as a primary solution.
ALBERT HENDERSHOT JR.
December 28, 2025 AT 11:33While the data suggests modest benefits, it remains essential to contextualize fusidic acid within a comprehensive treatment plan. 😊 Monitoring for local irritation and resistance is crucial.
Suzanne Carawan
January 3, 2026 AT 06:26Oh sure, because a 42 % reduction in lesion count is just a marketing gimmick, right? Let’s pretend no one benefits from a targeted topical.