Every year, millions of Americans take supplements - vitamins, herbs, probiotics, minerals - thinking they’re harmless. But here’s the truth: supplement interactions can be just as dangerous as mixing two prescription drugs. You might be taking St. John’s wort for mood, garlic pills for heart health, or calcium for bones, but if you’re also on blood thinners, antidepressants, or statins, you could be risking serious side effects - even hospitalization. And most people never tell their pharmacist.
Pharmacists aren’t just the people who hand out pills. They’re trained to spot hidden dangers in your medicine cabinet. A 2025 study found that only 3% of pharmacists initially caught a dangerous interaction between warfarin (a blood thinner) and a common avocado-soybean supplement. But when patients gave full details, that number jumped to over 12%. That’s not luck. That’s knowledge. And you have the power to unlock it.
Start with your list - every single thing you take
Before you walk into the pharmacy, grab a notebook or open a note on your phone. Write down everything you swallow, chew, or put under your tongue. Don’t leave anything out. That includes:
- Prescription medications (even if you’ve been on them for years)
- Over-the-counter drugs (ibuprofen, antacids, sleep aids)
- Dietary supplements (vitamin D, magnesium, fish oil, turmeric, etc.)
- Herbs and teas (ginger tea, chamomile, green tea extract)
- Probiotics and amino acids
- Any new product you tried because it was "all-natural" or "recommended by a friend"
For each item, note the brand, dose, and how often you take it. Example: "Ginkgo Biloba, 120 mg, once daily, Nature’s Bounty brand." Don’t say "I take a multivitamin." Say which one. Brands matter - some have more active ingredients than others.
Also, write down your daily eating habits. Do you eat grapefruit every morning? Drink milk with your meds? Eat a lot of leafy greens? Have a glass of wine at dinner? These aren’t just lifestyle choices. They’re part of your medication picture.
Ask the right questions - don’t wait for them to ask you
Pharmacists are busy. They won’t always ask about supplements unless you bring it up. Don’t assume they know. Say it clearly:
- "I’m taking St. John’s wort. Is it safe with my antidepressant?"
- "I started taking magnesium. Will that mess with my blood pressure pill?"
- "I eat grapefruit every day. Should I stop because of my cholesterol medicine?"
- "I take calcium supplements. Do I need to wait before I take my thyroid pill?"
Be specific. Don’t say "Do supplements interact with my meds?" That’s too vague. Pharmacists need details to give you real answers.
High-risk supplements to always mention:
- St. John’s wort - can make birth control fail, reduce effectiveness of antidepressants, and cause serotonin syndrome when mixed with SSRIs.
- Goldenseal - interferes with liver enzymes that break down over 50 common drugs, including blood thinners and diabetes meds.
- Ginkgo biloba - increases bleeding risk when taken with warfarin, aspirin, or NSAIDs.
- Garlic supplements - can thin blood and cause issues before surgery.
- Cranberry supplements - may boost warfarin’s effect, raising bleeding risk.
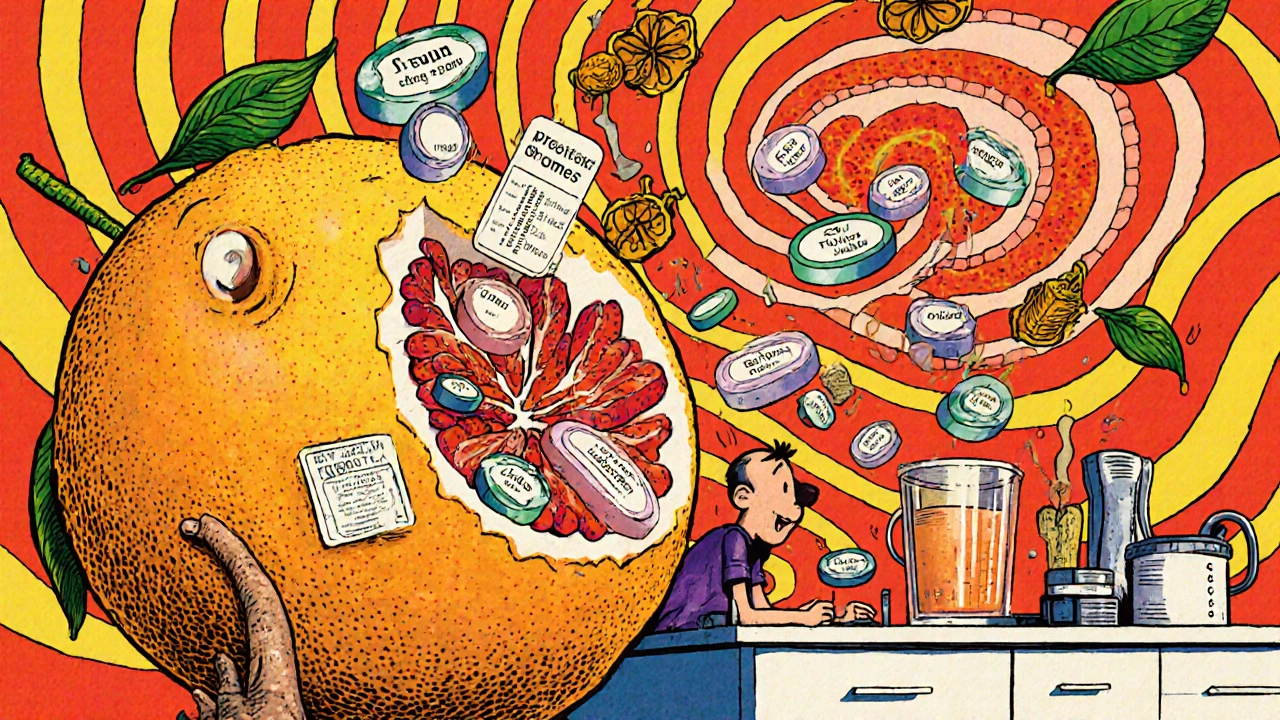
And don’t forget food. Grapefruit is the most well-known, but it’s not alone. Seville oranges, pomelos, and even some types of apple juice can interfere with statins, blood pressure meds, and anti-anxiety drugs. Dairy and calcium supplements can block absorption of antibiotics like tetracycline and thyroid meds. Wait at least 2 to 4 hours between these foods and your pills.
Know which meds deplete your nutrients
It’s not just about supplements interacting with drugs - drugs can also drain your body of essential nutrients. If you’re on one of these, you might be quietly deficient:
- Proton pump inhibitors (PPIs) - like omeprazole - deplete vitamin B12, magnesium, and calcium. Long-term use can lead to nerve damage and bone loss.
- Metformin - used for type 2 diabetes - lowers vitamin B12 and folate. This can cause fatigue, brain fog, and tingling in hands and feet.
- Statins - like atorvastatin - reduce coenzyme Q10. That’s linked to muscle pain and weakness, which many people blame on aging.
- Diuretics - water pills - flush out potassium and magnesium. That can lead to irregular heartbeat or cramps.
- Oral contraceptives - lower B vitamins and magnesium. This may contribute to mood swings and headaches.
If you’re on any of these, ask your pharmacist: "Should I be taking a supplement to replace what this drug is taking from me?" They can tell you which ones are proven to help - and which ones are just hype.
Supplements aren’t regulated like drugs - here’s what that means
The FDA doesn’t test supplements before they hit the shelf. That means what’s on the label isn’t always what’s inside. A 2023 study found that nearly 80% of herbal supplements didn’t contain the herb they claimed. Some had fillers, heavy metals, or even hidden prescription drugs.
Look for third-party seals: USP, NSF, or ConsumerLab. These organizations test for purity, potency, and contamination. If your supplement doesn’t have one, it’s a gamble. Tell your pharmacist what brand you use. They can check if it’s reliable.
Also, don’t assume "natural" means safe. Just because something comes from a plant doesn’t mean it won’t interact. St. John’s wort is a plant. So is foxglove - which contains digitalis, a heart drug. Nature doesn’t care if you’re trying to feel better. It just reacts.
Don’t stop or start anything on your own
Some people stop their meds because they start taking a supplement. Others quit the supplement because they heard it’s "bad." Both are risky.
Stopping statins suddenly can spike cholesterol. Stopping antidepressants cold turkey can trigger withdrawal. Suddenly adding a blood thinner like ginkgo can cause internal bleeding. Your pharmacist can help you adjust safely - if you tell them what you’re doing.
Even if you’ve been taking a supplement for years, it’s worth checking in. Your body changes. Your meds change. Your diet changes. What was safe last year might not be safe now.

Pharmacists are your most accessible health experts
Ninety-three percent of Americans live within five miles of a community pharmacy. You don’t need an appointment. You don’t need insurance. You can walk in during lunch, after work, or while picking up your prescription.
Many pharmacies now offer free 10-minute consultations just for supplement and interaction questions. Ask: "Can I speak with the pharmacist about my supplements?" If they say no, ask to speak with someone else. This is part of their job.
CVS, Walgreens, and other major chains updated their pharmacy systems in 2025 to flag potential supplement-drug interactions automatically. But the system only works if you tell them what you’re taking. If you don’t input it, they can’t warn you.
There’s a reason the American Pharmacists Association launched "Supplement Smart" in 2024 - because the problem is growing. With over 180 million Americans using supplements, and the market expected to hit $88 billion by 2028, pharmacists are stepping up. But they need your help to do it right.
What to do next
Here’s your simple action plan:
- Write down every supplement, herb, and food habit you have.
- Bring it to your next pharmacy visit - even if you’re just picking up a prescription.
- Ask: "Could any of these interact with my medications?"
- Ask: "Should I be taking anything to replace nutrients my drugs are draining?"
- Ask: "Is this brand reliable?" Show them the bottle.
- Don’t change anything until they say it’s safe.
You don’t need to be an expert. You just need to be honest. Your pharmacist isn’t judging you. They’re trying to keep you safe. And the more you tell them, the better they can help.
Supplements aren’t the enemy. Ignorance is. The right conversation can prevent a hospital trip, a stroke, or a dangerous drop in blood pressure. That’s not hype. That’s science. And it’s sitting right there in the pharmacy, ready to listen.

Jessica Healey
November 17, 2025 AT 22:38I took that ginkgo biloba for months without telling my pharmacist-thought it was just "natural" so it was fine. Then I got dizzy during yoga and nearly passed out. Turns out it was messing with my blood pressure med. My pharmacist looked at me like I’d just admitted to eating glitter. Never again. I now have a note in my phone labeled "PHARMACY LIST" and I update it like my life depends on it-because it does.
Levi Hobbs
November 19, 2025 AT 09:47Yes! Yes! Yes! I can't believe how many people think supplements are harmless because they're "natural"-that's like saying a rattlesnake is harmless because it's not a car. I'm a nurse, and I've seen patients come in with liver enzymes through the roof because they were taking "Turmeric for inflammation" while on statins. And they didn't even think to mention it. Please-write it down. Bring the bottle. Say it out loud. It's not embarrassing-it's lifesaving.
henry mariono
November 19, 2025 AT 23:50I appreciate this post. I've been on metformin for five years and never knew it was draining my B12. My hands have been tingling for months-I thought it was carpal tunnel. I'm going to ask my pharmacist next time I pick up my script. Thanks for the nudge.
Sridhar Suvarna
November 21, 2025 AT 14:38From India where herbal medicine is part of daily life I say this with respect: The West thinks supplements are new but we've been balancing herbs and drugs for centuries. The problem is not the supplement-it's the silence. In our villages, grandmas know which herb clashes with which pill. We must bring that wisdom into modern pharmacy. Not fear. Not hype. Just honest dialogue. Your pharmacist is not an enemy. They are the bridge.
Joseph Peel
November 21, 2025 AT 15:16The FDA doesn't regulate supplements? That's not a bug-it's a feature of American capitalism. Companies profit from ambiguity. Consumers pay in hospital bills. This isn't about personal responsibility-it's about systemic failure. We need mandatory labeling of active ingredients, third-party verification, and pharmacist-led screening built into every prescription refill. Until then, we're all playing Russian roulette with our liver enzymes.
Kelsey Robertson
November 23, 2025 AT 00:01Oh please. Another fear-mongering article from someone who thinks "natural" means "magic fairy dust"... St. John’s wort? It's been used for 2,000 years. Your antidepressants are synthetic poison. You're the one risking serotonin syndrome by mixing pharmaceuticals with other pharmaceuticals-supplements are just the scapegoat. Also, grapefruit? I've eaten it for 30 years. Still alive. Still sane. Still not on your meds.
Joseph Townsend
November 24, 2025 AT 18:11My mom took goldenseal because her friend’s yoga teacher said it "cleanses the liver"-then ended up in the ER with a drug interaction that looked like a sci-fi movie. The pharmacist had to call her cardiologist, her endocrinologist, AND her acupuncturist to untangle the mess. Now we have a family rule: No new supplement without a pharmacy consult. And we bring the bottle. Always. Because sometimes the bottle has more truth than the label.
Bill Machi
November 26, 2025 AT 14:02Why are we even talking about this? In America, we're too lazy to read the damn label. If you can't be bothered to know what's in your supplement, you don't deserve to take it. This isn't rocket science. It's basic hygiene. Stop blaming the pharmacist. Stop blaming the FDA. Take responsibility. Or don't take anything at all. Either way-stop wasting everyone's time.
Elia DOnald Maluleke
November 27, 2025 AT 02:12In my village in South Africa, we call this "the silence of the body"-when you take something and your body screams, but you pretend not to hear. The pharmacist is not a gatekeeper. They are the translator between your body and the chemicals you feed it. I once gave my uncle a herbal tea for his diabetes-he didn’t tell the doctor. Three weeks later, he was in ICU. The tea had hidden metformin. The pharmacist knew. But no one asked. The lesson? Speak. Even if your voice shakes.
satya pradeep
November 27, 2025 AT 04:40