Managing medications at home can feel overwhelming-especially when you're juggling multiple prescriptions, different times of day, and side effects that don’t make sense. For older adults, this isn’t just inconvenient-it’s dangerous. About 30% of all adverse events in home care come from medication errors. But there’s a proven solution: home health services for medication management.
What Home Health Services Actually Do for Medications
Home health services don’t just drop off pills. They create a safety net. Trained nurses or medication aides come to your home to make sure every pill is taken at the right time, in the right dose, and for the right reason. They check for duplicates, spot dangerous interactions, and update your list every time a doctor changes something. For example, if your cardiologist prescribes a new blood thinner and your primary care doctor didn’t know about it, a home health professional will catch that mismatch before it causes bleeding or a stroke. According to MedPro’s 2022 analysis, professional medication management cuts adverse drug events by 60% compared to self-management. These services are especially vital for seniors taking five or more medications-what doctors call polypharmacy. One in four older adults takes that many. And with each extra pill, the risk of confusion, missed doses, or harmful reactions goes up.How to Get Started with Home Health Medication Management
You don’t need a referral from a hospital to start. But you do need to know who qualifies. Medicare covers home health medication services if you meet three basic criteria:- You’re homebound (leaving home takes considerable effort or medical risk)
- You need skilled nursing care or therapy
- A doctor has ordered the services
- Ask your doctor for a home health referral. They’ll write an order and explain why you need it.
- Call a Medicare-certified home health agency in your area. You can find them through Medicare’s online provider directory.
- During the first visit, the nurse will review every medication you take-prescription, over-the-counter, vitamins, herbs. They’ll write it all down.
- You’ll get a personalized plan: when to take what, who to call if something goes wrong, and how to handle missed doses.
Tools That Make Medication Management Easier
No one remembers every pill at every time. That’s why tools matter. Pill organizers are the most common-and most effective. The Caregiver Action Network found they reduce errors by 45%. Look for ones with alarms, or ones that lock to prevent overuse. Some agencies, like Phoenix Home Care, use WellPack-individual daily pouches labeled with the time and medication name. No sorting needed. Just open and take. Digital tools help too. Apps like CritiCare’s digital planner send reminders and even require a fingerprint scan to confirm you took the dose. In pilot programs, that cut errors by 40%. And don’t underestimate simple tricks. Linking meds to daily habits-like brushing your teeth or eating breakfast-makes them stick. One study showed using meal times as cues improved adherence by 28%.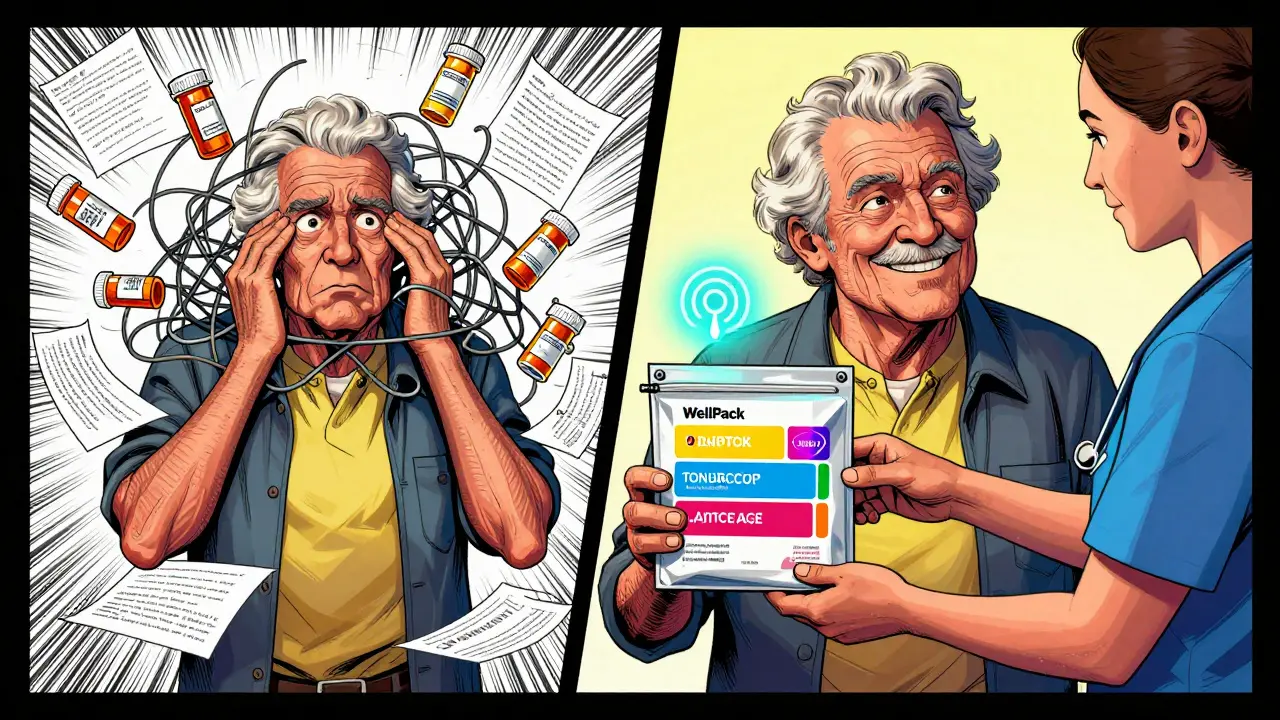
What to Look for in a Home Health Agency
Not all agencies are the same. Here’s what to ask:- Do they do full medication reconciliation at every visit? (This means comparing your current list to what your doctors prescribed.)
- Do they update your list in real time and share it with your doctors?
- Do they use the Beers Criteria to screen for risky medications in older adults?
- Can they speak your language? Many agencies now include QR codes that link to video instructions in 17 languages.
- What’s their process if you miss a dose? Do they have a 24/7 nurse line?
Real Stories: What Works and What Doesn’t
Mary K. from Ohio started using Phoenix Home Care’s WellPack system after her mother missed 30% of her doses. Within two weeks, missed doses dropped to under 5%. “It was like a weight lifted,” she said. But John T. from Reddit shared a scary story: his father had a dangerous interaction between blood thinners because two different doctors prescribed them, and no one told the home care team. He ended up in the ER. The fix? Better communication. A Clarest survey of 500 caregivers found 78% saw better adherence with home health help. But 42% struggled because specialists didn’t talk to each other. That’s why having one point person-the home health nurse-is so important.When Home Health Medication Management Falls Short
It’s not perfect. The biggest problem? Staff shortages. The National Association for Home Care & Hospice reports a 28% vacancy rate for home health nurses in 2023. That means longer wait times and fewer visits. Also, Medicare only covers intermittent care. If you need daily help for months, you’ll likely pay out of pocket. Some Medicare Advantage plans now cover continuous monitoring devices, but coverage varies. And for complex psychiatric meds-like lithium or antipsychotics-home health nurses aren’t always trained to adjust doses. That’s where a pharmacist or psychiatrist needs to step in.What’s Changing in 2026
The field is evolving fast. By 2025, 65% of agencies are expected to use AI tools that scan your meds for dangerous interactions in real time. Some are even testing wearable patches that confirm when a pill is taken. Medicare is also changing how it pays. Under its Value-Based Purchasing model, agencies get paid more if patients take their meds correctly-and less if they end up back in the hospital. That’s pushing agencies to get better. And cost savings? Real. Clarest’s 2023 study showed each patient saved about $1,200 a month in avoided ER visits and hospital stays.Final Checklist: Are You Getting the Most Out of Home Health Medication Services?
Use this quick list to make sure your care is on track:- ✅ You have a written, updated list of all meds-brand and generic names, doses, times, and why you take them.
- ✅ Your home health provider checks for duplicates and interactions every visit.
- ✅ You use a pill organizer or digital reminder system.
- ✅ Your nurse explains side effects in language you understand.
- ✅ You know who to call if you feel sick after taking a pill.
- ✅ Your doctor gets a copy of your updated med list every time it changes.
Can Medicare pay for home health medication management if I don’t need therapy?
Yes-but only if you’re homebound and need skilled nursing care. Medication management alone isn’t enough. You must also need something only a nurse can do, like wound care, IV therapy, or monitoring vital signs. If you only need help remembering pills, Medicare won’t cover it. But private agencies can help.
What if I miss a dose? Should I double up next time?
Never double up unless your doctor says so. Missing a dose is common, but doubling can be dangerous. Home health providers will give you a clear plan: if you miss a morning pill, take it as soon as you remember-if it’s still early. If it’s afternoon, skip it. They’ll also set up alerts so you’re less likely to miss it again.
How often should my medication list be updated?
Every time a doctor changes your meds-whether it’s a new prescription, a dose change, or something you stopped. Home health agencies are required to reconcile your list during every transition of care, like after a hospital stay. But you should also review it yourself every 30 days. Keep a copy in your wallet and share it with every provider.
Can home health nurses give me shots or IV meds at home?
Yes. Skilled home health nurses are trained to administer injections, IV antibiotics, chemotherapy, and other complex treatments. If you need these, make sure the agency you choose has nurses certified in those procedures. Not all do.
Are there free tools to help manage meds at home?
Yes. The National Institute on Aging offers a free printable medication tracker. Many pharmacies have apps that send refill reminders. Google Calendar can be set to alert you at specific times. But these tools work best when combined with human oversight. A nurse can catch what an app can’t-like a new symptom that means a drug isn’t working.
What if I don’t trust the home health nurse?
You have the right to request a different provider. Home health agencies must honor your preference. If you feel rushed, misunderstood, or unsafe, speak up. Ask for a supervisor. You’re not just a patient-you’re the boss of your care. If the agency won’t listen, call Medicare’s helpline or switch to another certified provider.

Susannah Green
January 22, 2026 AT 00:10Home health meds management changed my mom’s life-she was missing doses left and right, and the WellPack system? Absolute game-changer. No more confusion, no more panic when she’d forget if she took her blood pressure pill. The nurse came every Tuesday, checked everything, and even caught a duplicate prescription her cardiologist didn’t tell her PCP about. I wish I’d known about this sooner. It’s not just convenience-it’s survival.
Vanessa Barber
January 23, 2026 AT 11:2660% reduction in adverse events? Sounds like marketing fluff. I’ve seen home health nurses show up late, forget to update med lists, and one even gave my aunt the wrong dose because she was rushing. It’s not magic. People still die from errors-just slower now.
charley lopez
January 25, 2026 AT 05:47While the empirical data presented in this post is compelling, particularly the 60% reduction in adverse drug events per MedPro’s 2022 analysis, the operational feasibility remains contingent upon workforce availability. The 28% vacancy rate for home health nurses, as cited by NAHC, introduces significant systemic risk. Without addressing labor supply constraints, policy-level interventions may yield diminishing returns.
Anna Pryde-Smith
January 26, 2026 AT 12:09THIS IS A LIFESAVER. My dad almost died because two doctors gave him conflicting blood thinners and NO ONE TALKED TO EACH OTHER. I found out by accident when I saw his pill bottle. If you’re reading this and your loved one is on five or more meds-STOP WAITING. CALL A HOME HEALTH AGENCY TODAY. Don’t let bureaucracy kill them. I’m still angry about this. Don’t be like me.
Stacy Thomes
January 27, 2026 AT 16:08You got this! Seriously-every single person reading this deserves to feel safe taking their meds. Pill organizers? Yes. Alarms? Yes. A nurse who shows up and actually listens? DOUBLE YES. You’re not a burden. You’re a person who deserves to live well. Start today. One pill at a time. You’re not alone.
Dawson Taylor
January 28, 2026 AT 21:42Medication adherence is a function of systemic support, not individual willpower. The structural failure lies in the fragmentation of care delivery. A nurse’s visit cannot compensate for a lack of interprofessional communication. The solution requires institutional coordination, not merely supplemental labor.
Sallie Jane Barnes
January 28, 2026 AT 23:51I appreciate the thoroughness of this guide. However, I must emphasize that while Medicare coverage is invaluable, it is not universally accessible. Many seniors fall into the gap-homebound but not ‘skilled care eligible.’ Private agencies are often unaffordable. We need policy reform to expand eligibility beyond narrow clinical criteria. This is a civil rights issue.
Andrew Smirnykh
January 29, 2026 AT 11:24In my home country, Nigeria, many elderly rely on family members to manage meds. The idea of a professional coming to the house is rare-and expensive. But the principles here are universal: clarity, consistency, communication. I’ve translated parts of this for my cousin’s mother. Simple tools like pill boxes and meal-linked routines work everywhere. Culture changes, but human need doesn’t.
Kerry Evans
January 30, 2026 AT 04:05Everyone’s acting like this is groundbreaking. It’s not. People have been using pill organizers since the 80s. The real issue? Doctors who prescribe without checking what else the patient is on. Blame the prescribers, not the system. And don’t get me started on ‘digital tools’-my grandma can’t use an app that requires a fingerprint scan. That’s not innovation, that’s exclusion.
Kerry Moore
January 31, 2026 AT 06:37This is a thoughtful and comprehensive overview. I would only add that the emotional burden on caregivers should not be underestimated. The psychological relief provided by consistent, professional medication oversight is often as valuable as the clinical outcomes. Thank you for highlighting the human dimension alongside the data.
Sue Stone
February 1, 2026 AT 20:13I use the NIA printable tracker. Free, simple, and I print a new one every month. I keep it taped to the fridge next to the pill box. Works fine. No app needed.
Oladeji Omobolaji
February 3, 2026 AT 10:23My uncle in Lagos uses a plastic cup with different colored rubber bands for each day. He doesn’t even have a phone. But he remembers. Sometimes the simplest things work best. Technology helps-but it’s not the only way.
Janet King
February 5, 2026 AT 05:24Medicare’s requirement for skilled care eligibility excludes many who need medication management most. This policy gap is unacceptable. The definition of ‘skilled nursing’ must evolve to include complex polypharmacy oversight as a core competency, not an afterthought.
dana torgersen
February 6, 2026 AT 22:21ok so i read this whole thing and i think it’s amazing but… i think the part about the wellpack thing is kinda confusing? like, are they like little pouches? or like a box? and what if you can’t read? also i think the app thing is cool but my cousin’s grandma has shaky hands and she drops her phone all the time. just saying.
Laura Rice
February 7, 2026 AT 12:57My grandma used to take her meds at breakfast, lunch, and dinner-no organizer, no alarms. She’d say, ‘I know my body.’ Then she had a fall because she took her blood thinner after drinking grapefruit juice. We didn’t know. Now she has a nurse every Monday, Wednesday, Friday. She says, ‘I don’t feel like I’m carrying the whole world on my shoulders anymore.’ That’s what this is. Not a service. A peace of mind.