Hyponatremia Risk Calculator for SSRI Users
This calculator helps you understand your risk of developing hyponatremia (dangerously low sodium) when taking SSRIs. Based on the latest research, certain factors significantly increase your risk.
When you start an SSRI for depression, you expect better mood, more energy, maybe a good night’s sleep. But you might not expect to feel confused, dizzy, or nauseous - especially if you’re over 65. These aren’t just "normal aging" symptoms. They could be signs of something far more dangerous: hyponatremia - dangerously low sodium in your blood - triggered by the very medication meant to help you feel better.
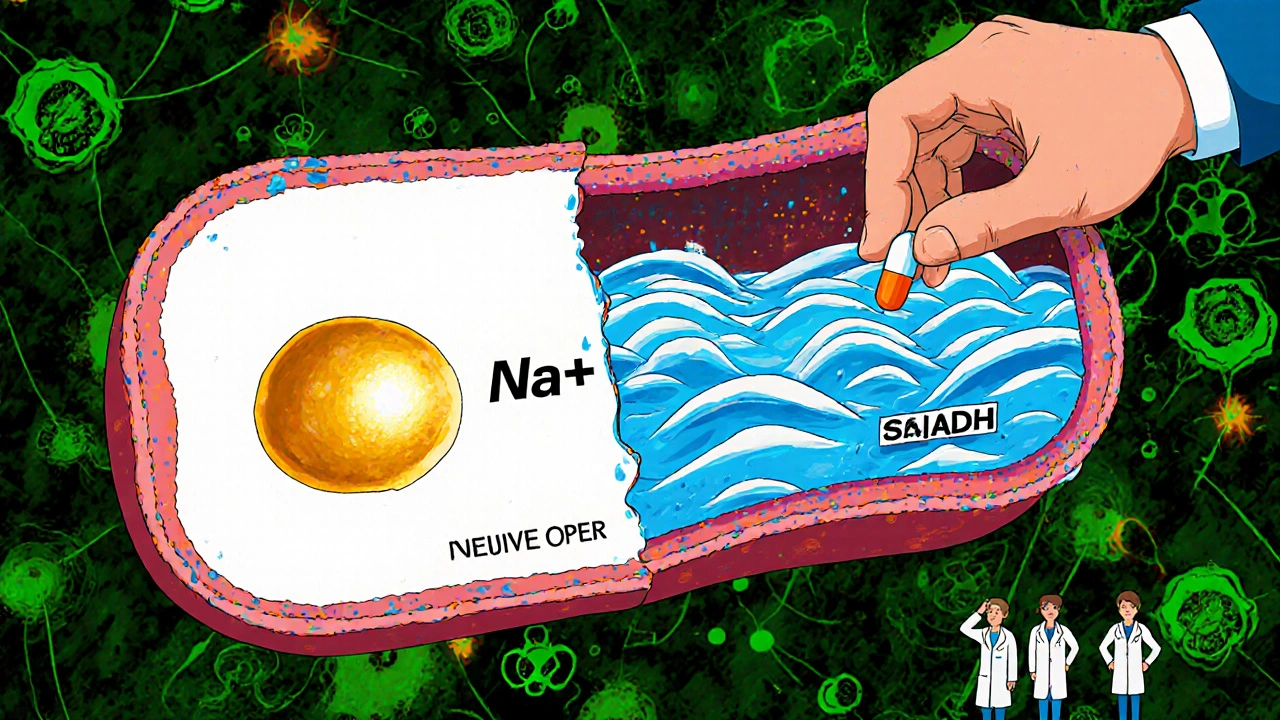
What Exactly Is Hyponatremia?
Hyponatremia means your blood sodium level has dropped below 135 mmol/L. Sodium isn’t just table salt. It’s a key electrolyte that helps your nerves, muscles, and brain work right. When sodium gets too diluted, your cells swell - especially brain cells. That’s when things get serious: confusion, seizures, coma, even death. Severe cases have seen sodium levels crash to 105-125 mmol/L. This isn’t rare. A 2024 meta-analysis found that nearly 1 in 25 people taking SSRIs develop this condition. For those over 65? It’s closer to 1 in 6.Why Do SSRIs Cause This?
It’s not the depression itself. It’s how SSRIs interact with your body’s water balance. These drugs boost serotonin - that’s how they lift mood. But serotonin also signals your brain to release antidiuretic hormone (ADH). Too much ADH means your kidneys hold onto water instead of flushing it out. The result? More water in your blood, diluted sodium. This is called SIADH - Syndrome of Inappropriate Antidiuretic Hormone Secretion. Not all SSRIs are the same. Citalopram and sertraline carry the highest risk. Fluoxetine and paroxetine follow close behind. Why? Because they bind tightly to the serotonin transporter (SERT). The stronger the binding, the more ADH gets released. It’s not just the drug - it’s how your body reacts to it.Who’s Most at Risk?
This isn’t a random side effect. Certain people are far more vulnerable:- Age 65+: Your kidneys don’t handle fluid the same way. Risk jumps to 13.9-18.6%.
- Women: Over 65% of reported cases are in women, likely due to body size and hormone differences.
- Low body weight (under 60 kg): Less total fluid means less buffer against dilution.
- Renal impairment: If your eGFR is below 60, your kidneys can’t clear excess water.
- On diuretics: Thiazide diuretics (like hydrochlorothiazide) increase risk by over 4 times.
- Rapid dose increases: Going from 10mg to 40mg of sertraline in a week? Big red flag.
Many people don’t realize they’re in the danger zone until it’s too late. That’s why doctors need to ask: Are you on a diuretic? Are you thin? Are you over 65? If yes, this isn’t just a routine prescription.
When Do Symptoms Show Up?
This isn’t a day-one side effect. Most cases show up between two and four weeks after starting the SSRI - or after a dose increase. That’s why so many cases get missed. A 78-year-old starts citalopram for sadness after losing her husband. Two weeks later, she’s forgetting names, stumbling, vomiting. Her family thinks it’s dementia. The doctor thinks it’s stress. But it’s hyponatremia. A simple blood test would’ve caught it.Symptoms start mild: headache, nausea, fatigue. Then come the red flags: confusion, disorientation, trouble walking, seizures. In elderly patients, these are often mistaken for Alzheimer’s or just getting older. But they’re not. They’re a medical emergency.
What Does the Science Say About Other Antidepressants?
SSRIs aren’t the only option. And some are much safer:| Medication | Risk Compared to SSRIs | Notes |
|---|---|---|
| Citalopram | 2.37x higher | Highest risk among SSRIs |
| Sertraline | 2.15x higher | Commonly prescribed, high risk |
| Fluoxetine | 1.98x higher | Long half-life, risk lingers |
| Mirtazapine | 0.47x (much lower) | Best alternative for elderly patients |
| Bupropion | 0.85x (low) | Doesn’t affect serotonin - safer choice |
| Venlafaxine (SNRI) | 1.72x higher | Still higher risk than mirtazapine |
| Amitriptyline (TCA) | 1.94x higher | Older drug, higher side effect burden |
Here’s the bottom line: If you’re over 65, or have kidney issues, or take a diuretic - mirtazapine is the safest antidepressant choice. It doesn’t trigger ADH release. It doesn’t cause hyponatremia at anything close to the same rate. The numbers don’t lie: for every 1,000 patients, SSRIs cause 18.6 cases of hyponatremia. Mirtazapine? Only 6.5. That’s a 65% lower risk.
What Should You Do Before Starting an SSRI?
You wouldn’t start a new heart medication without checking your blood pressure. Don’t start an SSRI without checking your sodium.- Get a baseline blood test within 7 days before starting the SSRI.
- Repeat the test at 2 weeks - that’s when levels start dropping.
- For high-risk patients (over 65, on diuretics, kidney problems), test monthly for the first 3 months.
Many primary care doctors don’t know this. A 2023 survey found that 63% didn’t know the typical onset window (2-4 weeks). If your doctor doesn’t mention testing, ask. Say: "I’ve heard SSRIs can cause low sodium. Can we check my levels before and after I start?"
What Happens If You Develop Hyponatremia?
If sodium is between 125-134 mmol/L and you’re not having seizures:- Stop the SSRI immediately.
- Restrict fluids to 800-1000 mL per day (no more than 3-4 cups).
- Recheck sodium in 24-48 hours. Most people recover fully in 3-4 days.
If sodium drops below 125 mmol/L - this is life-threatening. You need the hospital. Treatment involves slow, controlled IV saline to raise sodium no more than 6-8 mmol/L in the first 24 hours. Too fast, and you risk permanent brain damage called osmotic demyelination syndrome.
Recovery isn’t instant. One Reddit user shared that their 82-year-old mother spent 5 days in the hospital after citalopram dropped her sodium to 122. She was confused for weeks after. Her memory didn’t fully bounce back.
Why Is This Still Underdiagnosed?
Because symptoms look like other things. Confusion? Must be dementia. Nausea? Just a stomach bug. Fatigue? Old age. In 2023, only 28.7% of patients were told about this risk before starting SSRIs. That’s not informed consent - that’s negligence.And it’s expensive. In the U.S. alone, SSRI-induced hyponatremia costs $1.27 billion a year - mostly from ER visits and hospital stays. The FDA now requires SSRI labels to warn about this. But warnings don’t fix ignorance.
What’s Changing in 2025?
The tide is turning. Between 2018 and 2023, SSRI use in patients over 65 dropped 22%. Mirtazapine prescriptions for that group rose 35%. The American Geriatrics Society now lists SSRIs as "potentially inappropriate" for older adults. The European Medicines Agency is reviewing SSRI safety - results expected by fall 2025.By 2027, mirtazapine could be prescribed to over 40% of elderly patients needing antidepressants. That’s not a trend - it’s a correction.
Final Thoughts: Balance Risk and Benefit
SSRIs work. They save lives. But they’re not risk-free. In young, healthy adults, the chance of hyponatremia is low - maybe 1 in 50. The benefit of lifting depression often outweighs that risk. But for older adults, especially those on other meds or with kidney issues? The math flips.If you’re over 65, and your doctor suggests an SSRI, ask: "Is there a safer alternative?" Say "mirtazapine" or "bupropion." Don’t wait for confusion to set in. Don’t assume it’s just aging. Sodium levels can drop quietly - and dangerously - before you feel anything.
Ask for the blood test. Know the signs. Push for the right drug. Your brain deserves more than a guess.
Can SSRIs cause confusion in elderly patients?
Yes. Confusion is one of the most common early signs of hyponatremia caused by SSRIs. In older adults, this is often mistaken for dementia or normal aging. But it’s a medical reaction to low sodium levels in the blood - not a neurodegenerative disease. Symptoms like disorientation, memory lapses, and trouble speaking can appear within 2-4 weeks of starting the medication and should be evaluated immediately with a blood test.
Which SSRI has the lowest risk of causing hyponatremia?
Actually, all SSRIs carry significant risk. Citalopram and sertraline are the highest. Fluoxetine and paroxetine are also high-risk. There is no SSRI with a low risk of hyponatremia. For patients over 65 or with kidney issues, doctors should consider switching to mirtazapine or bupropion - antidepressants that don’t trigger the same hormone response and have far lower rates of sodium imbalance.
How long does it take for hyponatremia to develop after starting an SSRI?
Most cases develop between 2 and 4 weeks after starting the medication or after a dose increase. This timing is critical because symptoms often appear after the first follow-up appointment, so many cases go unnoticed. That’s why repeat sodium testing at 2 weeks is now considered standard for older adults and high-risk patients.
Is hyponatremia from SSRIs reversible?
Yes, if caught early. Stopping the SSRI and restricting fluids usually brings sodium levels back to normal within 3-4 days. But if sodium drops below 125 mmol/L and is corrected too quickly, it can cause permanent brain damage called osmotic demyelination syndrome. Slow, careful correction under medical supervision is essential.
Should I stop my SSRI if I feel confused?
Don’t stop abruptly without talking to your doctor - sudden withdrawal can cause its own problems. But if you’re confused, dizzy, nauseous, or having headaches after starting an SSRI, especially if you’re over 65, call your doctor immediately. Get a blood test for sodium levels. Don’t wait. This is not something to monitor at home.
Can I take a diuretic with an SSRI?
Combining a diuretic (like hydrochlorothiazide) with an SSRI increases your risk of hyponatremia by more than 4 times. This combination is dangerous, especially for older adults. If you’re on both, your doctor should be monitoring your sodium levels monthly. In many cases, switching to a non-SSRI antidepressant like mirtazapine is the safest solution.
What to Do Next
If you’re taking an SSRI and you’re over 65, on a diuretic, or have kidney disease:- Ask for your last sodium level.
- Ask if you need another test in the next two weeks.
- Ask if mirtazapine or bupropion might be a safer option.
- If you’ve been feeling off - confused, tired, nauseous - don’t brush it off. Get tested.
This isn’t about avoiding antidepressants. It’s about choosing the right one - safely. Your mental health matters. So does your sodium. Don’t let one save you while the other puts you at risk.

gina rodriguez
November 28, 2025 AT 16:08Thanks for sharing this. I’ve been worried about my mom starting sertraline after her husband passed. I didn’t realize how common this was. I’m going to ask her doctor for a sodium test before she starts. Better safe than sorry.
Sue Barnes
November 29, 2025 AT 04:45This is why I tell everyone: doctors are lazy. They hand out SSRIs like candy. My aunt ended up in the ER with sodium at 118 because her GP never mentioned testing. It’s not just negligence-it’s criminal. If you’re over 65, don’t trust a pill without proof.
jobin joshua
November 30, 2025 AT 21:03Bro this is wild 😱 I’m from India and my grandma was on citalopram for 3 months and kept forgetting my name. We thought it was dementia… turns out it was hyponatremia. We switched to mirtazapine and she’s back to her old self. 🙏
Sachin Agnihotri
December 1, 2025 AT 08:52Wow, this is such an important post-seriously, why isn’t this in every primary care pamphlet? I’m a nurse, and I’ve seen so many elderly patients get misdiagnosed with ‘just aging’ when it’s actually SIADH from SSRIs. The 2-4 week window is everything. I always tell my patients: if you feel off after starting a new med, get bloodwork. No excuses.
Diana Askew
December 1, 2025 AT 17:11Big Pharma doesn’t want you to know this. They profit off confusion, hospital stays, and long-term care. They knew SSRIs caused this for years. They buried the data. The FDA? Bought and paid for. This isn’t medicine-it’s a scam. Check your sodium or die. That’s the real choice they give you.
King Property
December 3, 2025 AT 16:35Everyone’s acting like this is news. I’ve been screaming this since 2018. Citalopram? High risk. Sertraline? High risk. Mirtazapine? Safe. Bupropion? Safe. The science is settled. If your doctor doesn’t know this, they’re not qualified to prescribe antidepressants. Period. Stop trusting ‘general practitioners’-go see a psychopharmacologist. Or better yet, don’t take anything unless you’ve read the FDA label yourself.
Pawittar Singh
December 4, 2025 AT 10:12Hey everyone, I’m a geriatric nurse in Delhi and I’ve seen this over and over. 💔 Elderly patients on SSRIs + diuretics? That’s a time bomb. I always push for mirtazapine-it’s gentle, works great for sleep and mood, and doesn’t mess with sodium. I’ve had families cry with relief when we switch. You’re not giving up on treatment-you’re choosing safety. 🙏 Let’s stop normalizing brain fog as aging.
Josh Evans
December 5, 2025 AT 18:35My dad was on fluoxetine for a year before he started zoning out at dinner. We thought he was just tired. Turned out his sodium was 124. He spent a week in the hospital. Now he’s on bupropion and feels like himself again. Honestly, if I’d known this earlier, I could’ve saved him a lot of fear and confusion.
Allison Reed
December 7, 2025 AT 16:30This is exactly the kind of information that needs to be more widely known. Thank you for laying it out so clearly. The fact that 63% of doctors don’t even know the typical onset window is terrifying. We need better education-not just for patients, but for the entire medical system. This isn’t just about one drug; it’s about how we approach mental health in older adults. You’ve done a real service here.
Jacob Keil
December 9, 2025 AT 01:13the real issue here is not the ssri or the sodium… it’s the entire paradigm of modern medicine. we treat symptoms not causes. depression isn’t a chemical imbalance-it’s a spiritual wound. but no one wants to hear that. so we give pills and call it progress. the hyponatremia? just a side effect of our collective denial. 🤷♂️
Rosy Wilkens
December 10, 2025 AT 17:42How is it possible that this is still not mandatory protocol? This is not a suggestion-it’s a life-or-death risk. And yet, insurance companies won’t cover pre-prescription labs. Doctors don’t have time. Patients don’t know. It’s a perfect storm of corporate greed and systemic failure. This is why I refuse to take any psychiatric medication without a full electrolyte panel-and I’m not even elderly. If you’re not demanding this, you’re complicit.
Andrea Jones
December 11, 2025 AT 04:56So… you’re saying my therapist’s ‘just try sertraline’ was basically playing Russian roulette with my mom’s brain? 😅 Thanks for the reality check. I’m printing this out and handing it to her doctor tomorrow. Maybe he’ll actually read it this time.
Justina Maynard
December 12, 2025 AT 08:00Imagine being 72, grieving your spouse, and the one thing meant to help you feel human makes you forget your own daughter’s face. That’s not mental illness-that’s a pharmacological betrayal. And the worst part? No one bats an eye until you’re in a hospital gown, confused, and surrounded by machines. We’ve turned healing into a gamble. And the house always wins.
Evelyn Salazar Garcia
December 12, 2025 AT 20:28Ugh. Another long post. Just don’t take SSRIs if you’re old. Done.