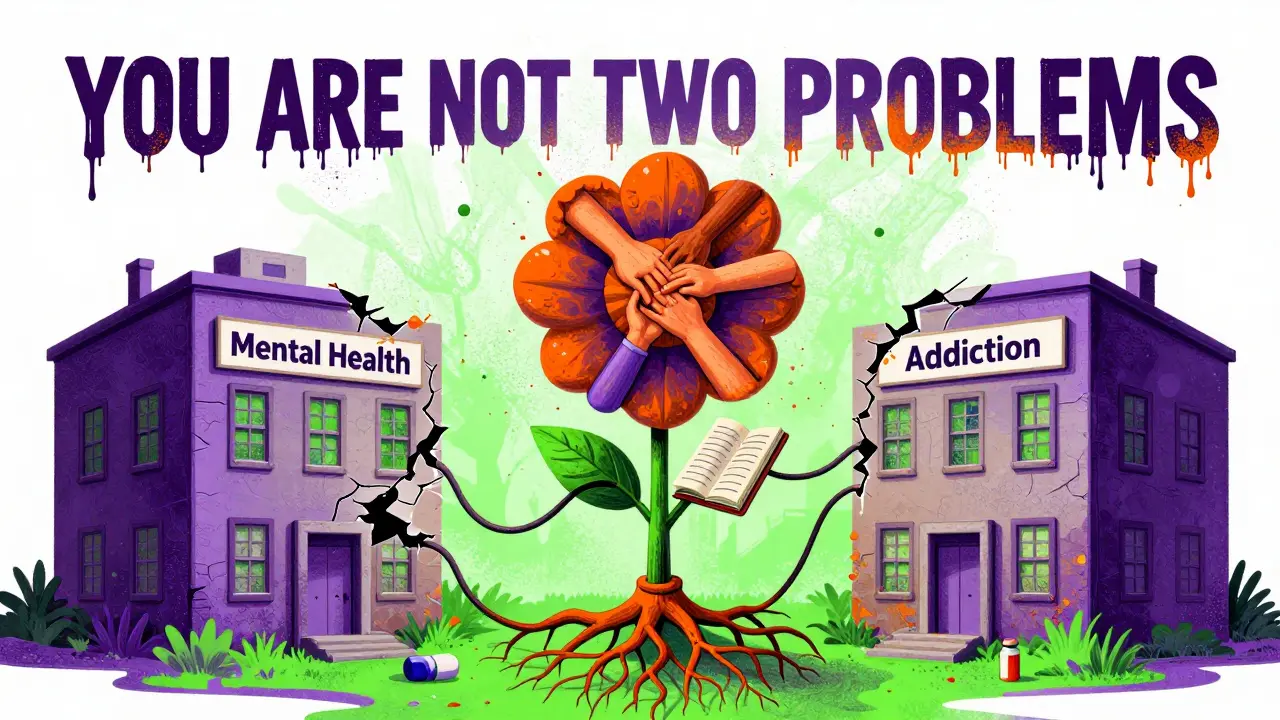
Imagine needing help for depression and alcohol use at the same time. You walk into a mental health clinic, and they give you therapy for your mood. Then you’re told to go across town to a different building for addiction counseling. No one talks to the other team. Your meds aren’t coordinated. You feel like you’re juggling two separate problems - when really, they’re tangled together. This isn’t rare. It’s the norm for millions of people. And it’s broken.
Why Dual Diagnosis Isn’t Two Problems - It’s One
About 20.4 million U.S. adults live with both a mental illness and a substance use disorder. That’s not a coincidence. Depression, anxiety, PTSD, bipolar disorder - these don’t just happen alongside addiction. They feed each other. Someone with untreated schizophrenia might use alcohol to quiet the voices. Someone with severe anxiety might start using opioids to feel calm. Then, the substance makes the mental illness worse. The brain changes. The symptoms multiply. The cycle tightens. Traditional treatment treated these as separate issues. One clinic for mental health. Another for addiction. Patients bounced between them. Many dropped out. Why? Because when you’re struggling with psychosis or suicidal thoughts, showing up to a second appointment feels impossible. And if your counselor doesn’t understand how your trauma fuels your drinking, they can’t help you stop. Integrated Dual Diagnosis Treatment (IDDT) changes that. It’s not a new drug or a fancy app. It’s a simple idea: one team. One plan. One path forward. The same clinician helps you manage your schizophrenia and your cocaine use. The same group session talks about coping with panic attacks and avoiding triggers. The same medication review considers how your antidepressant interacts with your alcohol use. No more confusion. No more blame. Just care that matches your reality.How IDDT Works - The Nine Core Pieces
IDDT isn’t just a buzzword. It’s a structured model with nine proven components, developed by researchers at Dartmouth and refined over decades. Here’s what it actually looks like on the ground:- Motivational interviewing: Not about pushing abstinence. It’s about asking, "What do you want your life to look like?" and helping people move toward that - even if they’re still using.
- Substance abuse counseling: Focuses on reducing harm, not just stopping. If someone can’t quit drinking yet, the goal is to cut down on binge episodes, avoid driving, and stop using before therapy sessions.
- Group treatment: People with co-occurring disorders sit together. They learn from each other’s struggles with mood swings, cravings, and social isolation.
- Family psychoeducation: Loved ones aren’t left out. They learn how to support without enabling, how to recognize early signs of relapse, and why yelling doesn’t help.
- Self-help group participation: Encourages connection to groups like Dual Recovery Anonymous, where people don’t have to choose between "I’m an addict" or "I’m mentally ill." They’re both.
- Pharmacological treatment: Medications are chosen with both conditions in mind. Antipsychotics that don’t worsen anxiety. Mood stabilizers that don’t interact dangerously with alcohol.
- Health promotion: Physical health is part of recovery. Sleep, nutrition, exercise - these aren’t "nice to haves." They’re tools to stabilize the brain.
- Secondary interventions: For people who aren’t responding, the team adjusts. Maybe they need more frequent check-ins. Or a different therapy. Or housing support.
- Relapse prevention: Not a one-time lecture. It’s a living plan: What happens if you start hearing voices again? What do you do if your friend offers you a drink? What’s your exit strategy?
This isn’t theory. It’s practice. And it works - but only when done right.
What Makes IDDT Different From Parallel Treatment
Parallel treatment means two separate systems. Two sets of paperwork. Two sets of rules. Two different messages. One counselor says, "Stop using." The other says, "Your anxiety is the problem." Who do you believe? IDDT flips that. It says: "Your substance use and your mental illness are connected. We’ll treat them together." The results? A 2018 study of 154 patients found a significant drop in days of alcohol and drug use after IDDT. People spent fewer nights in emergency rooms. Fewer jail stays. Fewer hospitalizations. But here’s what most people miss: IDDT doesn’t always make depression disappear overnight. It doesn’t always fix relationships. It doesn’t magically give someone a job. Those are secondary goals. The core win? People stay in treatment longer. They feel heard. They don’t have to explain their whole life twice. And that’s what keeps them alive.
The Hard Truth: Why IDDT Isn’t Everywhere
If IDDT works so well, why are only 6% of people with co-occurring disorders getting it? Because it’s expensive. It’s complicated. And the system isn’t built for it. Most clinics are funded to treat one thing at a time. Mental health clinics get paid for therapy sessions. Addiction centers get paid for detox and group meetings. No one gets paid to do both - and do them well. Staff need training. Not a one-day workshop. Real, ongoing education. Clinicians must understand how antipsychotics affect dopamine pathways. How trauma impacts addiction recovery. How to talk to someone who’s suicidal and still using heroin. That takes time. And money. A 2018 study trained 37 clinicians in IDDT over three days. The result? No improvement in their skills. No change in their ability to do motivational interviewing. The training was too short. Too superficial. And then there’s the funding gap. Washington State’s 2023 analysis showed IDDT reduces substance use symptoms - but the cost to run it outweighs the savings. For every dollar spent, only 50 cents in benefits are returned. That doesn’t make sense to administrators who are told to cut budgets. So most places stick with the broken system. It’s cheaper in the short term. But it costs more in the long run - in ER visits, homelessness, incarceration, and death.Who Benefits Most From IDDT?
IDDT isn’t for everyone. But it’s life-changing for people with:- Severe mental illness - schizophrenia, bipolar disorder, major depression with psychosis
- Chronic substance use - alcohol, opioids, stimulants
- A history of failed treatment - multiple rehab stays, hospitalizations, lost jobs
- Homelessness or unstable housing
- Justice system involvement
These are the people who fall through the cracks. The ones who get labeled "non-compliant" or "treatment-resistant." But they’re not broken. The system is.
IDDT gives them a chance. Not because it’s perfect. But because it doesn’t pretend they have to be perfect to get help.
What Recovery Looks Like in IDDT
Recovery doesn’t mean quitting everything on day one. In IDDT, recovery means:- Getting up in the morning - even if you drank last night
- Attending your therapy session - even if you’re scared
- Taking your meds - even if you don’t feel like it
- Calling your counselor when you feel like using - not after you’ve already used
- Knowing you’re not alone - because your team knows your whole story
One patient in a Portland-based IDDT program told his team: "I used to think I had to choose between being sober or being stable. Now I know I can work on both at the same time. I’m not failing. I’m learning." That’s the shift.
What’s Next? The Road to Wider Access
The Substance Abuse and Mental Health Services Administration (SAMHSA) has been pushing for IDDT since the 2000s. They fund training, technical support, and state grants. But real change needs more than federal wishes. It needs:- Payment reform: Medicaid and Medicare must pay for integrated care as a single service - not split it into two.
- Workforce investment: Train more clinicians. Pay them fairly. Support ongoing education.
- Co-location: Put mental health and addiction services under one roof. Same building. Same receptionist. Same chart.
- Community partnerships: Work with housing agencies, job centers, and courts to wrap support around people.
The goal isn’t to fix everyone. It’s to give people a real shot. To stop treating them like two separate problems. To say: "You’re not broken. The system is. And we’re fixing it."
There are over 15 million people in this country who need this care and aren’t getting it. They’re not waiting for miracles. They’re waiting for someone to listen - all at once.
What is integrated dual diagnosis treatment (IDDT)?
Integrated Dual Diagnosis Treatment (IDDT) is a structured, evidence-based approach that treats both mental illness and substance use disorders at the same time, by the same team of providers. Unlike traditional models that separate care, IDDT combines counseling, medication, family support, and harm reduction into one unified plan to address the full picture of a person’s health.
How is IDDT different from regular therapy or rehab?
Regular therapy or rehab often treats one condition at a time. You might go to a mental health clinic for depression, then drive across town for addiction counseling - with no communication between the two teams. IDDT eliminates that gap. One provider understands both your anxiety and your opioid use. One treatment plan addresses both. This reduces confusion, builds trust, and improves outcomes.
Do I have to quit drugs completely to get IDDT?
No. IDDT uses a harm reduction approach. That means the focus is on reducing the negative consequences of substance use - like avoiding overdose, staying off the streets, or not using before therapy - even if complete abstinence isn’t possible yet. The goal is progress, not perfection. Many people reduce use over time, and some eventually stop. But the treatment starts where you are.
Is IDDT only for people with severe mental illness?
IDDT was originally designed for people with serious mental illnesses like schizophrenia, bipolar disorder, or major depression with psychosis - especially when combined with chronic substance use. But the model is being adapted for other co-occurring conditions, including anxiety disorders and PTSD with alcohol or stimulant use. The key is whether the two conditions interact and worsen each other.
Why isn’t IDDT available everywhere?
Most healthcare systems are funded to treat mental health and addiction as separate services. Insurance doesn’t pay for integrated care the same way. Clinics lack trained staff, funding for ongoing training, and physical space to combine services. It’s more expensive upfront - even though it saves money long-term by reducing ER visits, jail time, and hospitalizations.
Can family members be involved in IDDT?
Yes. Family psychoeducation is one of the nine core components of IDDT. Loved ones learn how mental illness and addiction affect each other, how to support without enabling, and how to recognize early signs of relapse. This reduces conflict, builds safety, and helps the whole family heal.
How effective is IDDT?
Studies show IDDT significantly reduces days of alcohol and drug use and improves treatment retention. One 2018 study found patients used substances fewer days per month after IDDT. It doesn’t always fix mood symptoms or social functioning right away - but it keeps people alive, engaged, and moving forward. The biggest win? People stay in treatment longer - and that’s what leads to lasting change.
Where to Find IDDT Services
IDDT is growing, but access is still limited. Look for:- Assertive Community Treatment (ACT) teams that mention co-occurring disorders
- Community mental health centers with substance use counselors on staff
- Programs funded by SAMHSA’s Co-Occurring Center of Excellence
- State health departments with "co-occurring disorders" or "dual diagnosis" programs
If you’re unsure, call your local mental health authority or ask your primary care provider. Demand integrated care. If they don’t offer it, ask why - and push for change. Because no one should have to choose between healing their mind and healing their body.

Faith Wright
January 11, 2026 AT 15:35So let me get this straight-we spend billions on jail and ER visits because we can’t be bothered to put two clinics in the same building? Brilliant. I’m sure the guy sleeping under the bridge with bipolar and a bottle of cheap whiskey really appreciates the efficiency of our healthcare system. 😏
Jose Mecanico
January 13, 2026 AT 00:25I’ve seen this work in a small clinic in Ohio. One team, one chart, one person who actually remembers your name. It’s not magic-it’s just basic human decency. The data doesn’t lie, even if the funding does.
George Bridges
January 13, 2026 AT 10:00As someone who grew up in a community where mental health and addiction were whispered about, seeing IDDT implemented felt like a quiet revolution. No one had to choose between being ‘broken’ or ‘weak.’ They just got help. It’s not perfect, but it’s the first time I’ve seen the system try to meet people where they are.
Darryl Perry
January 14, 2026 AT 06:12This is just socialist healthcare dressed up in clinical jargon. We don’t need another bureaucracy. People should just stop using drugs and get therapy. Simple.
Abner San Diego
January 15, 2026 AT 05:31Oh great, another ‘integrated’ program that costs more than it saves. Why not just lock them up? At least then taxpayers don’t have to fund their rehab while they binge on opioids and forget to take their lithium. America’s problems aren’t medical-they’re moral.
Eileen Reilly
January 15, 2026 AT 22:26ok so like… i work in a clinic and we tried this thing called IDDT and honestly? it’s a mess. staff are burnt out, the software doesn’t talk to the other system, and half the patients don’t show up anyway. why are we pretending this works? it’s just feel-good policy with no real funding. also, who writes this like a textbook? 🙄
TiM Vince
January 17, 2026 AT 14:30In my country, we don’t separate mental health and addiction care because we don’t see them as separate. It’s not about ideology-it’s about biology. The brain doesn’t have separate drawers for trauma and addiction. It just hurts. And when you treat the hurt, not the label, people heal.
gary ysturiz
January 18, 2026 AT 19:42This is the kind of care that saves lives. Not because it’s fancy, but because it’s real. People aren’t broken. They’re just trying to survive. And when you give them a team that sees the whole picture? That’s hope.
Jessica Bnouzalim
January 20, 2026 AT 15:58I’m a mom whose son was in and out of rehabs for 5 years… until we found IDDT. He’s been sober for 18 months. He still takes his meds. He still has bad days. But now? He has a team that knows his whole story. I cried the first time his counselor asked about his anxiety AND his drinking in the same sentence. Thank you for writing this.
Bryan Wolfe
January 21, 2026 AT 01:00One of my clients told me last week: ‘I used to think I had to choose between being sober or being stable.’ Now he says, ‘I’m learning.’ That’s the whole point. You don’t have to be perfect to deserve help. You just have to be human. And this model? It lets you be that.