Steroid Injection Risk Calculator
Your Injection History
Enter details about your steroid injections to assess your risk level
Your Risk Assessment
For decades, steroid injections into joints have been a go-to fix for knee, hip, and shoulder pain. Millions of people get them every year-around 12 million in the U.S. alone-because they work fast. If your knee hurts from osteoarthritis, a shot can calm the inflammation and get you walking again in days. But here’s the part no one talks about enough: steroid joint injections aren’t harmless. They don’t just stay in the joint. They leak into your bloodstream. And that’s where things get risky.
How Steroid Injections Actually Work (and Why They Don’t Stay Local)
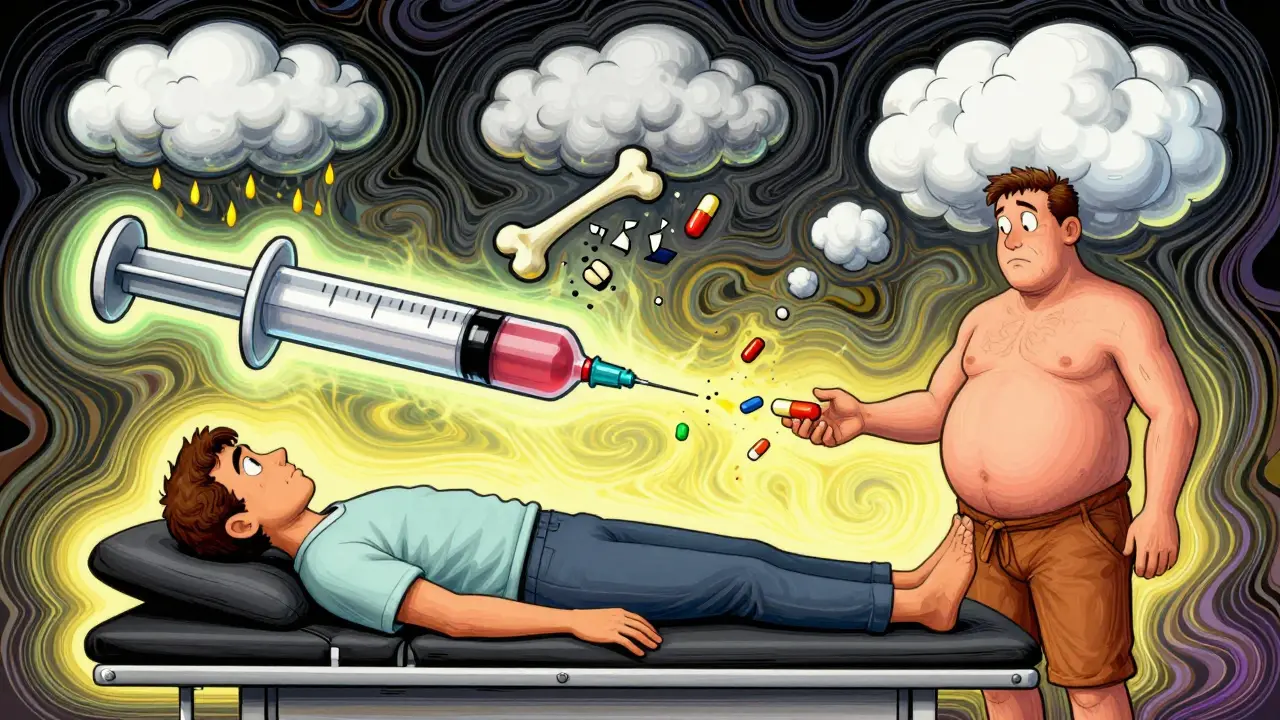
The idea behind these injections is simple: put the medicine right where it’s needed. Corticosteroids like triamcinolone acetonide, methylprednisolone, or betamethasone are powerful anti-inflammatories. When injected into a joint, they should reduce swelling and pain without affecting the rest of your body. That’s the promise. But reality doesn’t always match the promise. Studies show these drugs don’t stay put. Triamcinolone, one of the most common types used, gets absorbed into the bloodstream more than others. Once it’s in your blood, it acts like an oral steroid-even if you never swallowed a pill. That means your adrenal glands, your blood sugar, your bones, and even your cartilage are all exposed to the same powerful hormones that were meant to target only your knee or hip.The Hidden Risks: More Than Just a Temporary Flare
Most people know about the short-term stuff: a little pain after the shot, maybe a flushed face, or a spike in blood sugar if you’re diabetic. Those usually fade in a day or two. But the long-term risks are quieter-and far more damaging. A 2023 study in Radiology followed hundreds of patients who got steroid injections for osteoarthritis. What they found shocked many doctors: people who got these shots were more likely to see their joints get worse over time. Not just painful-actually deteriorating. Joint space narrowed by 2 millimeters or more in just 12 months. That’s not normal wear and tear. That’s accelerated destruction. The same study linked steroid injections to:- Subchondral insufficiency fractures-tiny cracks in the bone under the cartilage
- Osteonecrosis-bone tissue dying because blood flow gets cut off
- Rapid progressive osteoarthritis-where the joint breaks down much faster than it should
Systemic Side Effects You Can’t See
Your joint isn’t the only place these steroids go. Once they enter your blood, they affect your whole body. Here’s what can happen:- High blood sugar-Even if you don’t have diabetes, a steroid shot can spike your glucose levels for days. For diabetics, this can mean hospital visits or insulin adjustments.
- Adrenal suppression-Your body makes its own cortisol. When you get repeated steroid shots, your adrenal glands forget how. That can lead to fatigue, low blood pressure, and even life-threatening crashes if you get sick or injured.
- Bone loss-Steroids weaken bones. Postmenopausal women, older adults, and anyone on long-term steroids are at higher risk for osteoporosis and fractures.
- Fluid retention and high blood pressure-Steroids make your body hold onto salt and water. That raises blood pressure and can strain your heart.
- Cushing-like symptoms-Weight gain around the midsection, thinning skin, easy bruising, and mood swings can show up even after just a few injections.
Who Should Avoid These Injections?
Not everyone should get them. Some people are at much higher risk:- People with early-stage osteoarthritis-If your X-ray shows only mild changes but you’re in a lot of pain, the problem might not be arthritis. A steroid shot could mask something worse and speed up joint damage.
- Diabetics-Your blood sugar control can unravel after a shot. Monitor closely for at least a week.
- Postmenopausal women-Bone density is already declining. Steroids make it worse.
- People planning surgery-Steroids weaken tissue healing. Getting a shot within 3-6 months before joint replacement can increase complications.
- Anyone with a history of infection-Steroids suppress your immune system. A shot could turn a small skin infection into a deep joint infection.
What Do the Guidelines Really Say?
You’ll hear doctors say, “It’s safe if you don’t do it too often.” That’s what the guidelines say too-usually no more than 3 to 4 times a year per joint. But that’s not based on hard proof. It’s based on tradition. The American Academy of Orthopaedic Surgeons still conditionally recommends these injections for knee osteoarthritis. But the same group that made that recommendation also published a 2023 review saying we need to rethink this. Why? Because the evidence is changing. Dr. Ali Guermazi, who led the landmark 2023 study, put it plainly: “We’ve been telling patients that even if these injections don’t relieve your pain, they’re not going to hurt you. But now we suspect that this is not necessarily the case.” Other studies disagree. Some show no difference in joint damage between people who got shots and those who didn’t. But those studies often looked at short-term outcomes. The real damage takes years to show up on X-rays or MRIs. The truth? The science isn’t settled. But the warning signs are clear enough to pause and think twice.
Alternatives That Actually Protect Your Joints
If you’re looking for pain relief without the risk, there are better options:- Physical therapy-Strengthens muscles around the joint, reduces stress on cartilage. Studies show it works as well as steroids for knee pain-with no side effects.
- Weight loss-Losing just 10 pounds cuts knee pain by 50% in overweight people. It’s the most effective treatment for osteoarthritis.
- Bracing or orthotics-Helps redistribute pressure away from damaged areas.
- Platelet-rich plasma (PRP) or hyaluronic acid injections-Still being studied, but they don’t carry the same systemic risks as steroids. PRP may even help repair tissue.
- Low-impact exercise-Swimming, cycling, walking. Movement keeps joints lubricated and strong.
What to Do If You’ve Already Had a Shot
If you’ve had one or two steroid injections and are feeling fine, don’t panic. But do take action:- Track how many you’ve had and when. Keep a record.
- Ask your doctor to check your bone density if you’re over 50 or postmenopausal.
- If you’re diabetic, monitor your blood sugar for 7-10 days after each shot.
- Don’t schedule another shot unless you’ve tried at least two non-steroid options first.
- Get a follow-up X-ray or MRI in 6-12 months if you’ve had more than one injection.
Are steroid joint injections safe for people with diabetes?
Steroid injections can cause significant spikes in blood sugar, even in people without diabetes. For those with type 1 or type 2 diabetes, blood glucose levels can remain elevated for up to 10 days after the injection. It’s critical to monitor glucose closely during this time and adjust insulin or oral medications as needed under medical supervision. Some endocrinologists recommend avoiding these injections entirely in poorly controlled diabetics.
How many steroid injections are safe per year?
Most guidelines suggest no more than 3 to 4 injections per joint per year. But this limit is based on tradition, not proven safety. Evidence shows that even two injections in a year can increase joint damage over time. The real question isn’t how many-you should ask whether you need any. Alternatives like physical therapy or weight management are safer and often just as effective.
Can steroid injections cause permanent joint damage?
Yes. Studies have shown that repeated steroid injections can accelerate cartilage loss, trigger bone fractures under the joint surface, and lead to rapid joint destruction. These changes are often irreversible. Once the joint space narrows significantly or bone dies from osteonecrosis, the only option may be joint replacement surgery. The damage doesn’t always show up right away-it can take months or years to become visible on imaging.
Do steroid injections work better for some joints than others?
Steroid injections tend to work best in larger, simpler joints like the knee or shoulder. In smaller joints like those in the hands or feet, the risk of tissue damage and infection is higher, and the benefit is often shorter-lived. For hips, the evidence is mixed-some studies show faster joint deterioration after injection, while others don’t. The location matters, but the systemic risks apply to all joints.
What should I do if I experience pain after the injection?
A mild increase in pain for 24 to 36 hours after the shot is common-it’s called a steroid flare and usually resolves on its own. But if the pain is severe, the joint swells up, feels hot, or you develop a fever, that’s not normal. It could be an infection or a reaction to the steroid. Seek medical care immediately. Septic arthritis, though rare, is a medical emergency that can destroy a joint in days if untreated.
Is there a safer alternative to corticosteroid injections?
Yes. Platelet-rich plasma (PRP) and hyaluronic acid injections are two alternatives with fewer systemic risks. PRP uses your own blood to stimulate healing and may slow cartilage loss. Hyaluronic acid lubricates the joint and can provide relief for months. Physical therapy and weight loss are even safer and have stronger long-term evidence. While they don’t work as fast as steroids, they protect your joint instead of damaging it.

Uzoamaka Nwankpa
January 5, 2026 AT 02:05The more I read about these injections, the more I realize how much we’ve been sold a myth. It’s not just about pain relief-it’s about systemic sabotage, and no one talks about it until it’s too late. I’ve seen friends go from walking without aid to needing a cane in under two years after a few ‘harmless’ shots. The medical community is still in denial.
Jennifer Glass
January 5, 2026 AT 03:33I’m a physical therapist and I see this every day. Patients come in after their third steroid shot wondering why their knee is worse than before. We spend months rebuilding strength they could’ve preserved if they’d just started with PT instead of a needle. The system rewards quick fixes, not long-term health.
melissa cucic
January 6, 2026 AT 20:04It’s astonishing how deeply entrenched this practice is-despite mounting evidence. The American Academy of Orthopaedic Surgeons’ conditional recommendation feels less like science and more like institutional inertia. We’ve normalized a treatment that accelerates degeneration because it’s convenient for the patient, the provider, and the payer. But convenience isn’t care.
Oluwapelumi Yakubu
January 7, 2026 AT 05:09Let me tell you something, my friends-steroid shots are the pharmaceutical equivalent of putting duct tape on a crumbling bridge. You think you’ve fixed it? Nah. You’ve just delayed the inevitable collapse while pretending everything’s fine. Meanwhile, your bones are whispering for help, and your adrenal glands? They’ve already filed for divorce.
Abhishek Mondal
January 7, 2026 AT 17:45Actually, the data is far more nuanced than this article suggests. Several randomized controlled trials-including the 2021 JAMA study by Smith et al.-found no statistically significant difference in joint space narrowing between steroid and saline groups at 24 months. The Radiology study you cite? Small sample size, selection bias, and confounding by indication. Also, cartilage loss on MRI doesn’t always correlate with clinical symptoms. You’re conflating radiographic change with functional decline.
Chris Cantey
January 8, 2026 AT 03:24There’s a deeper truth here, one that transcends medicine: we’ve outsourced our responsibility for health to a needle. We want the miracle, not the磨难. We crave the instant fix because we’ve forgotten how to suffer with patience, how to move through discomfort as a teacher rather than an enemy. The body doesn’t break because of steroids-it breaks because we’ve stopped listening to it.
Terri Gladden
January 9, 2026 AT 08:38OMG I just had my 3rd knee shot last week and now I’m terrified!! I’ve been having weird mood swings and my face is puffy!! I didn’t know this could happen!! I’m gonna cancel my next one and start walking my dog every day!!
Aaron Mercado
January 9, 2026 AT 11:47People who get these injections are just lazy. If you can’t manage your weight, do PT, or live a healthy lifestyle, then you deserve the damage. This isn’t a medical issue-it’s a moral one. Stop expecting your body to be fixed by a shot while you sit on the couch eating chips. Take responsibility!
mark etang
January 10, 2026 AT 10:23As a board-certified rheumatologist with over 25 years of clinical experience, I must respectfully challenge the alarmist tone of this article. While systemic absorption of intra-articular corticosteroids is documented, the clinical significance of subclinical metabolic changes in otherwise healthy patients is negligible. The benefits of pain relief, functional improvement, and delay of surgical intervention overwhelmingly outweigh the theoretical long-term risks-especially when used judiciously. The notion that two injections can cause irreversible joint destruction is not supported by large-scale longitudinal data. We must avoid therapeutic nihilism. Evidence-based medicine requires nuance, not fear.