Every year, more than 1.5 million people in the U.S. end up in the emergency room because of medication mistakes. Many of these errors are preventable - and the biggest reason they happen? Patients don’t know the right questions to ask. You don’t need to be a doctor to protect yourself. You just need to know a few key terms and how to use them when you’re handed a new prescription, told to take a shot, or given a pill at the hospital.
What Are the Eight Rights of Medication Safety?
The foundation of medication safety isn’t a complicated algorithm or a high-tech app. It’s a simple list called the Eight Rights. These aren’t suggestions - they’re checkpoints that can stop a dangerous mistake before it happens. You’ve probably heard of the original Five Rights. But today, experts agree: you need all eight.
- Right patient: They must confirm your identity with two things - your full name and date of birth. Don’t let them skip this, even if they’ve seen you before. Hospitals mix up patients every day.
- Right medication: Ask for both the brand name and the generic name. If your doctor says "Lipitor" and the label says "atorvastatin," that’s the same thing. But if you’re handed something you didn’t expect, speak up.
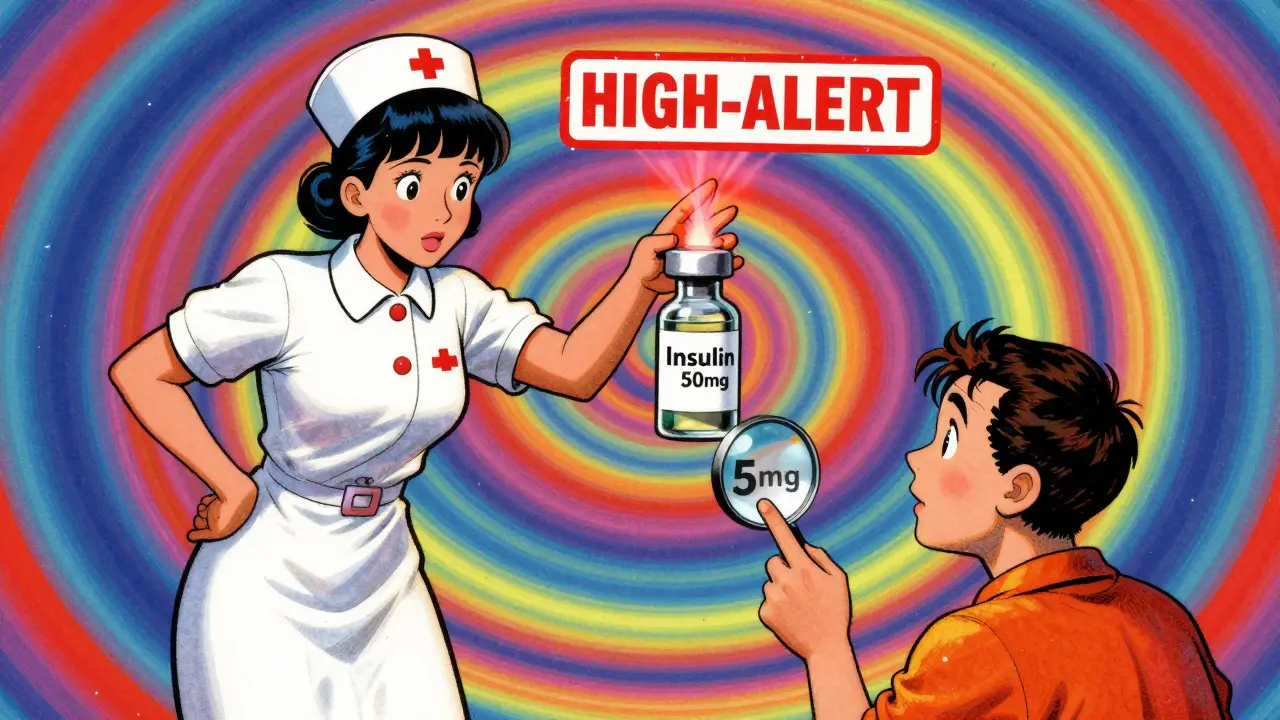
- Right dose: Is it 5 mg or 50 mg? That’s a tenfold difference. For kids, this is even more critical - 15% of pediatric errors happen because someone misread the dose. Always ask: "How much is this, and why this amount?"
- Right route: Is this pill meant to be swallowed, placed under the tongue, injected into the vein, or applied to the skin? Giving an IV drug by mouth can kill you. If you’re unsure, ask: "How is this supposed to go into my body?"
- Right time: Are you supposed to take this with food? Every 8 hours? At bedtime? Timing matters. Taking blood pressure meds at night instead of morning can make them less effective. Use your phone to set reminders.
- Right reason: This is the most powerful one. Ask: "Why am I taking this?" If your doctor says "for pain," but you have no pain, that’s a red flag. Studies show patients who ask this reduce wrong prescriptions by 28%.
- Right documentation: Did they write it down? Did they update your chart? If you’re discharged from the hospital and handed a new list of meds, compare it to what you were taking before. If something’s missing or added without explanation, ask why.
- Right response: What should you feel? What side effects are normal? What’s dangerous? If you’re on a blood thinner and start bruising easily, that’s not normal. Track how you feel. Write it down. Bring it to your next appointment.
What Is an Adverse Drug Event (ADE)?
An adverse drug event isn’t just a side effect. It’s any harm caused by a medicine - whether it’s because you took too much, the wrong one, or it reacted badly with something else. The CDC says ADEs are one of the top causes of preventable hospital visits. And they’re not rare.
Think of it this way: if you take a new antibiotic and get a rash, that’s a side effect. But if that rash turns into a life-threatening allergic reaction? That’s an ADE. If you take two painkillers that both contain acetaminophen and end up with liver damage? That’s an ADE. If your blood pressure drops too low because you forgot to tell your doctor you’re on a diuretic? That’s an ADE.
Knowing this term gives you power. When you say, "I think I’m having an adverse drug event," doctors take it seriously. They don’t brush it off as "just a side effect." You’re not being difficult - you’re being smart.
What Are High-Alert Medications?
Some medicines are more dangerous than others. These are called high-alert medications. They’re not necessarily strong - they’re just unforgiving. A small mistake with one of these can kill you.
The Institute for Safe Medication Practices (ISMP) lists these as high-alert:
- Insulin
- Blood thinners like warfarin or rivaroxaban
- Opioids like morphine or oxycodone
- Chemotherapy drugs
- Intravenous potassium chloride
- IV sedatives like midazolam
These drugs account for 67% of fatal medication errors. That’s not a guess - it’s data from thousands of reported errors. If you’re prescribed one of these, you need to be extra careful. Ask: "Is this a high-alert drug? What happens if I take too much? What should I watch for?"
And never assume the pharmacist or nurse knows you’re on another one. If you’re taking warfarin and your doctor prescribes a new antibiotic, ask: "Will this interact with my blood thinner?"
What’s a Close Call?
A close call is when something almost went wrong - but didn’t. Maybe the nurse caught the wrong dose before giving it. Maybe the pharmacist noticed the wrong label. Maybe you asked, "Wait, I thought this was for my back pain?" - and they stopped to check.
Close calls are the quiet heroes of medication safety. They don’t make headlines. But they happen all the time. And if you’re the one who spotted the error? You just saved yourself.
Don’t think of a close call as "luck." Think of it as proof that asking questions works. If you’ve ever said, "That doesn’t look right," and someone paused to double-check - you did your part. Keep doing it.
What Are Sentinel Events?
A sentence event is the worst-case scenario: a death or serious injury caused by a medication error. The Joint Commission - the group that sets hospital safety standards - defines these as events that should never happen. And they happen more than you think.
One common sentinel event? Giving a patient the wrong drug because the labels looked similar. Like confusing "hydralazine" (for high blood pressure) with "hydroxyzine" (for allergies). They sound alike. They look alike. And people die from this mix-up every year.
If you’re hospitalized, ask: "What are you doing to prevent errors?" Hospitals that track sentinel events and train staff on the Eight Rights have 40% fewer medication errors. You have the right to know.

Why Does This Matter Right Now?
In 2024, the Joint Commission made it official: hospitals must teach patients these terms before discharge. The CDC and FDA want 90% of patients to know at least five of these terms by 2030. Why? Because it works.
Patients who use these terms reduce their risk of harm by up to 50%. That’s not hype. That’s from studies by the American College of Obstetricians and Gynecologists. People who ask about the right reason for their meds cut down on wrong prescriptions by 37%. Those who track side effects reduce severe reactions by 35%.
And it’s not just about pills. It’s about power. When you use these words - "right patient," "high-alert," "adverse event" - you’re not being annoying. You’re speaking the language of safety. And healthcare workers respect that.
How to Start Using These Terms Today
You don’t need to memorize everything at once. Start with three:
- Always ask: "What is this medicine for?" (Right reason)
- Always ask: "Is this the right dose?" (Right dose)
- Always ask: "What side effects should I watch for?" (Right response)
Write them down. Put them on your phone. Say them out loud. The first time you ask, it might feel awkward. The second time, it’ll feel normal. The third time? You’ll wonder why you didn’t do it sooner.
And if you’re helping a parent, an elderly relative, or someone with low health literacy - teach them these terms. Explain them like you’re talking to a friend. Use simple words. No jargon. Just facts: "This medicine is for your heart. If you feel dizzy, call your doctor. Don’t wait."
What If You Don’t Understand?
Only 12% of U.S. adults have strong health literacy. That means most people struggle with medical terms. That’s not your fault. But it’s your responsibility to ask for help.
Here’s what to do:
- Ask for a translator if English isn’t your first language. Hospitals are required to provide one.
- Ask for a printed handout. If they don’t have one, ask if they can email it.
- Bring someone with you to appointments. A second set of ears helps.
- Use free apps like Medisafe - they remind you when to take pills and check for interactions.
You’re not alone. Millions of people are learning this right now. And every time you speak up, you make it easier for the next person.

Steve Hesketh
January 21, 2026 AT 08:08Yo this is the kind of stuff I wish my grandma knew before she got hospitalized last year. She took two different painkillers that both had acetaminophen and ended up in the ER with liver damage. No one told her to check the labels. If she’d known about ADEs and high-alert meds, she’d still be cooking her jollof rice instead of recovering in a hospital bed. Share this with everyone you know - especially older folks. This ain’t just info, it’s survival.
And yeah, the Eight Rights? I printed them out and taped them to my fridge. Now I ask every doc, ‘What’s the right reason?’ Like it’s my job. And guess what? They start treating me like a partner, not a patient.
shubham rathee
January 21, 2026 AT 14:58So the government wants us to memorize these terms because they’re too lazy to fix the system. Hospitals mix up names? Yeah because they hire people who can’t read. Insulin errors? Because they use handwritten scripts. This whole thing is just putting the burden on the patient instead of fixing broken infrastructure. I’m not here to be a medical detective. I’m here to get better. Why should I have to be the one asking if this is a high-alert drug? That’s their job.
Also I think they meant sentinel event not sentence event. Probably typo. But still. This feels like a PR stunt.
Sangeeta Isaac
January 22, 2026 AT 16:39Okay but can we talk about how the word ‘right’ is used like 80 times in this post? Like ‘right patient right medication right dose right route right time right reason right documentation right response’ - it’s a tongue twister and also a corporate slogan. I love the intent but it reads like a PowerPoint slide that got too excited.
Also I’m 32 and I still don’t know what ‘right documentation’ means. Did they mean ‘did they update your chart?’ Yeah okay cool but why not just say that? Why make it sound like a military checklist? I’m not deploying a drone I’m taking a pill.
Also I just Googled ‘hydralazine vs hydroxyzine’ and holy hell they look like twins. I’m terrified now. Thanks for that.
Alex Carletti Gouvea
January 24, 2026 AT 01:34This is why America is falling apart. We’re turning patients into medical auditors. Back in my day you trusted your doctor. Now you gotta interrogate them like they’re a suspect in a crime show. You want safety? Fix the damn system. Don’t make every Joe on the street memorize eight rights like it’s the Ten Commandments. We got enough laws already.
And who’s paying for these apps and translators? Not me. I work two jobs. I don’t have time to be your medical advocate. Just give me the damn pill and let me go.
Uju Megafu
January 25, 2026 AT 07:56Okay so let me get this straight - you’re telling me that if I take a blood thinner and my doctor prescribes an antibiotic without checking interactions, that’s not negligence? That’s MY fault for not asking? And if I die? That’s just a ‘sentinel event’? Like it’s some kind of tragic poetry?
I’ve been in three hospitals. Three. And every single time, the nurses rolled their eyes when I asked questions. One even said ‘You’re being difficult.’ So now I’m supposed to be brave and speak up? In a system that punishes people for being alert?
This isn’t empowerment. It’s gaslighting with a checklist.
lokesh prasanth
January 26, 2026 AT 20:38Right patient right medication right dose. All these rights mean nothing if the system is designed to fail. The real right is the right to not be treated like a liability. We are not customers. We are bodies in a machine. The machine doesn’t care if you know the eight rights. It cares about quotas and billing codes. This post is beautiful. But it’s a bandaid on a severed artery.
MARILYN ONEILL
January 28, 2026 AT 02:33I work in healthcare. I’ve seen this. People don’t ask questions because they’re scared. Or they’re tired. Or they don’t think they matter. But this list? It’s gold. I give it to every new patient. Even the ones who roll their eyes. I say ‘Say these three words: What is this for? What if I miss a dose? What should I watch for?’ And guess what? They start remembering. They start feeling less helpless.
It’s not about being a know-it-all. It’s about being alive. And if you think this is too much to ask - you’ve never been the person who almost died because someone assumed you knew what you were taking.
Coral Bosley
January 29, 2026 AT 10:45I had a close call last month. Got handed a prescription for ‘metoprolol’ but the label said ‘metformin’. I didn’t know the difference. But I knew the bottle looked wrong. I called my pharmacist. Turned out the pharmacy had swapped two bottles in the same drawer. They apologized. Gave me a gift card. But I didn’t feel like a hero. I felt like I narrowly avoided a funeral.
That’s why I keep a list in my wallet now. Not for the doctors. For me. Because if I don’t speak up, no one else will. And I’m tired of being a statistic.
MAHENDRA MEGHWAL
January 29, 2026 AT 21:08While the intent of the article is commendable and aligns with established patient safety protocols endorsed by the WHO and ISMP, it is imperative to recognize that the efficacy of such knowledge is contingent upon systemic accessibility. In regions where healthcare infrastructure is under-resourced or linguistic barriers persist, the burden of cognitive labor imposed upon patients may exacerbate existing inequities. A patient’s ability to interrogate clinical decisions is not universally enabled by information alone, but requires institutional support, time, and psychological safety. The Eight Rights are not merely a checklist; they are a social contract between caregiver and cared-for - one that cannot be upheld by the latter alone.