When you or a loved one is given a new medication, the stakes are high. One wrong dose, one misunderstood instruction - and the result can be hospitalization, organ damage, or worse. Now imagine trying to understand those instructions in a language you don’t speak well. That’s the reality for millions of people in the U.S. every day. Language barriers aren’t just an inconvenience - they’re a direct threat to medication safety.
Why Language Barriers Lead to Dangerous Mistakes
A 2022 study from the Children’s Hospital of Philadelphia found that children in families with limited English proficiency had nearly double the rate of medication errors compared to English-speaking families: 17.7% versus 9.6%. These aren’t small mistakes. They’re missed doses, wrong amounts, or taking the wrong drug altogether. One mother in Portland told her story: her Spanish-speaking mother was given insulin instructions on a printed sheet translated by Google Translate. It said “1 unit” when it meant “10 units.” She took the wrong dose. She ended up in the ER. This isn’t rare. Nearly half of all adults with limited English proficiency (LEP) report facing a language barrier during a healthcare visit within three years, according to a 2023 KFF survey. And when it comes to prescriptions, the problem gets worse. A Milwaukee study found that about half of pharmacies never or only sometimes provide written instructions in languages other than English. Even when they do, the translations are often incomplete or inaccurate. Terms like “dropperful,” “take with food,” or “for thirty days” don’t always translate correctly - and patients don’t know enough to ask for clarification.What Happens When Family Members Interpret
It’s tempting to rely on a child, cousin, or friend to translate. But research shows this is one of the riskiest choices you can make. Up to 25% of interpretations done by untrained family members contain serious errors - not just mispronunciations, but missing key medical terms like “hypertension,” “allergic reaction,” or “do not crush.” In one case documented by the Patient Safety Network, a grandmother used her grandson to interpret a new blood thinner prescription. The boy translated “take once daily” as “take when you feel sick.” She took it only when she had chest pain - skipping days, then doubling up. She ended up with internal bleeding. A trained interpreter would have caught the confusion before it started. The problem isn’t just about language. It’s about context. Family members don’t know medical terminology. They might skip scary words to avoid worrying someone. Or they might add their own advice - “I think you should take it at night,” or “My cousin took this and got sick.” These aren’t clinical facts. They’re guesses. And in medication safety, guesses cost lives.What Works: Professional Interpreters and Direct Observation
The best solution isn’t fancy tech or expensive software. It’s trained, certified medical interpreters - in person, over the phone, or via video. Studies show that using professional interpreters can cut medication error rates by up to 50% for LEP patients. That’s not a guess. That’s from data collected across thousands of cases. In one hospital in Seattle, after switching from using staff who spoke a little Spanish to certified medical interpreters, medication errors among Spanish-speaking patients dropped by 40% in just one year. The same hospital started using a “teach-back” method: after explaining the medication, the provider asks the patient to repeat the instructions in their own words. If the patient can’t explain it clearly, they keep practicing until they can. Simple. Effective. Another powerful tool is directly observed dosing - especially for high-risk drugs like insulin, blood thinners, or seizure medications. A nurse or pharmacist watches the patient take the first dose. They watch them open the bottle, measure the liquid, swallow it. If there’s confusion - even a pause, a frown, a hesitant hand - they stop and clarify. No translation needed. Just observation. A 2017 study in the Journal of General Internal Medicine showed this method improved accuracy even when language barriers were present.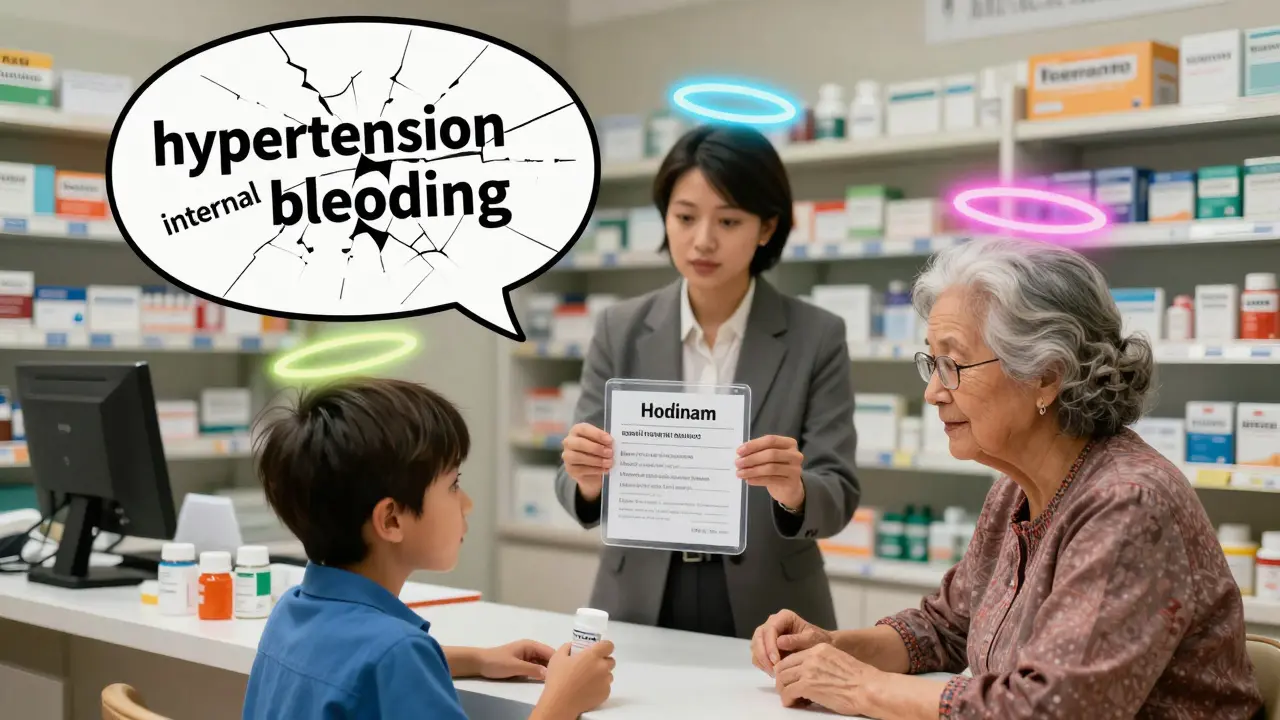
What Pharmacies and Clinics Should Be Doing
By law, any healthcare provider receiving federal funds - which includes nearly every hospital, clinic, and pharmacy in the U.S. - must provide language assistance under Title VI of the Civil Rights Act. That means they’re required to offer free interpreter services. But compliance is patchy. Here’s what effective systems look like:- Universal language identification: Every patient is asked at check-in: “What language do you speak best?” Not just once - every time.
- Professional interpreters for all clinical interactions: No exceptions for “quick questions.” Medication instructions are clinical interactions.
- Translated medication labels and instructions: Prescription labels should include the drug name, dose, frequency, and purpose in the patient’s language. Not just a translated version of the English label - a culturally adapted one.
- Staff training: Nurses, pharmacists, and front desk staff need to know how to request an interpreter, how to work with one, and why it matters. Training takes 4-8 hours, but it saves lives.
What You Can Do as a Patient or Caregiver
You don’t have to wait for the system to fix itself. Here’s how to protect yourself or your loved one:- Ask for an interpreter: Say, “I need a professional interpreter. I don’t feel comfortable relying on family.” You have the right to one.
- Ask for written instructions in your language: If the pharmacy says they can’t print it, ask for a printed version from the doctor’s office. Or ask if they can email it to you in your language.
- Use the teach-back method: After the provider explains the medication, say: “Can you help me explain this back to you so I’m sure I got it right?”
- Take the first dose with someone who speaks English: If you’re starting a new drug, ask a friend or neighbor who speaks English to be there when you take it. Have them watch you measure it, read the label, and confirm the instructions.
- Report problems: If you’re given wrong instructions or denied an interpreter, report it. Call the clinic’s patient advocate. File a complaint with the Office for Civil Rights. Your voice matters.

The Bigger Picture: Why This Isn’t Just About Language
This isn’t just about translation. It’s about equity. When a Spanish-speaking grandmother gets the wrong dose of blood pressure medicine because the label was poorly translated, it’s not an accident. It’s a system failure. The same system that gives clear, printed instructions to English speakers denies that same clarity to others. The U.S. population is changing. By 2030, one in four Americans will speak a language other than English at home. If we don’t fix this now, the problem will only grow. And the cost? Not just dollars - lives. The Quality Health analysis estimated that communication failures in healthcare cost the system $1.7 billion annually in avoidable harm. But change is possible. The FDA is planning new rules in 2024 to require clearer multilingual labeling on prescriptions. Medicare now pays for video interpreter services during telehealth visits. Hospitals are starting to integrate language preferences directly into their electronic records. These are steps forward.What’s Next
If you’re a patient or caregiver, start today. Ask for an interpreter. Ask for written instructions. Don’t assume someone else will fix it. If you’re a provider, pharmacist, or clinic manager, audit your current practices. Do you know how many of your patients have limited English? Do you have a plan to reach them? Is your pharmacy system capable of printing labels in Spanish, Chinese, or Somali? If not, start there. Medication safety isn’t just about the drug. It’s about the message. And if the message doesn’t get through - because of a language gap - then the medicine might as well be useless.Can I use Google Translate for medication instructions?
No. Google Translate and other free apps are not reliable for medical instructions. They often mistranslate dosing terms, miss context, and can’t handle medical jargon. A 2022 Reddit user shared that their mother was hospitalized after using Google Translate to understand insulin instructions. The app confused “1 unit” with “10 units.” Always ask for a professional interpreter or written materials in your language.
Are interpreters free?
Yes. Under Title VI of the Civil Rights Act, any healthcare provider receiving federal funding - which includes most hospitals, clinics, and pharmacies - must provide free interpreter services. You do not have to pay. If someone asks you for money or says it’s not available, ask to speak to a supervisor or patient advocate.
What if I speak a less common language like Hmong or Somali?
Even for less common languages, professional interpretation services are available through phone or video platforms like LanguageLine or Certified Languages International. These services offer interpreters for over 200 languages. It may take a few extra minutes to connect, but it’s still available. Don’t accept “we don’t have someone for that” as an answer - ask to be connected to their language services coordinator.
How do I know if my pharmacy can provide translated labels?
Ask directly: “Can you print my prescription label in [your language]?” If they say no, ask if they can email it to you or provide a printed version from the doctor’s office. You can also request an interpreter to explain the label to you in person. If they refuse, file a complaint with the Office for Civil Rights at HHS.gov.
What is teach-back, and how does it help?
Teach-back is when a provider asks you to explain back in your own words what you’ve been told. For example: “Can you tell me how you’ll take this pill?” This helps catch misunderstandings before they cause harm. It’s not a test - it’s a safety tool. Use it every time you’re given new medication instructions.

Crystel Ann
January 14, 2026 AT 14:40It’s terrifying how many people assume translation apps are safe for medical use. I’ve seen grandparents take insulin wrong because of a Google Translate glitch - and no one takes responsibility. This isn’t just about language. It’s about dignity.
Niki Van den Bossche
January 15, 2026 AT 00:07Let’s be brutally honest: the healthcare system doesn’t care if you understand your meds - it only cares that you sign the waiver. The real tragedy isn’t the mistranslated label - it’s that we’ve normalized this as ‘just how it is’ for non-English speakers. We’ve turned linguistic exclusion into a business model disguised as bureaucracy.
Every time a pharmacist says, ‘We don’t have someone for Somali,’ they’re not being resource-limited - they’re complicit. The system isn’t broken. It was designed this way.
Teach-back? That’s not a solution. That’s a Band-Aid on a severed artery. What we need is a complete overhaul of how language is valued - or rather, devalued - in clinical spaces. Until then, we’re just rearranging deck chairs on the Titanic while people drown in pill bottles.
And yes, I’ve watched my aunt nearly die because the ‘interpreter’ was the 14-year-old cousin who thought ‘hypertension’ meant ‘high energy.’
Stop calling this a ‘language barrier.’ It’s a moral failure dressed in policy.
Nat Young
January 16, 2026 AT 04:30Let’s not romanticize this. The study says medication errors drop 50% with interpreters? That’s still a 50% failure rate. And who’s to say those interpreters aren’t just as likely to botch ‘do not crush’ as a teenager with Google Translate? Data doesn’t lie - but it doesn’t tell the whole story either.
Also, why are we assuming all non-English speakers want interpreters? Maybe some just want to figure it out themselves. Maybe they’re proud. Maybe they’ve survived 40 years without ‘professional’ help and don’t need a cultural consultant to hold their hand.
And let’s talk about the ‘teach-back’ method - it’s just a way for providers to shift responsibility onto the patient. ‘Can you explain this back?’ What if they don’t trust the system? What if they’re afraid to admit they didn’t understand? That’s not safety - that’s performative compliance.
Also, why is everyone ignoring the fact that many of these patients are undocumented? They don’t want to be ‘identified’ at check-in. They’re terrified. The system isn’t failing them - it’s actively hunting them.
Jami Reynolds
January 17, 2026 AT 12:06It’s no coincidence that the same hospitals that refuse to provide interpreters are the ones receiving federal grants for ‘health equity.’ This is a manufactured crisis to funnel money into language services contractors - many of whom are owned by the same private equity firms that own the hospitals. The real issue isn’t translation - it’s profit.
Google Translate isn’t the villain. The villain is the $2.3 billion industry built around ‘medical interpretation services’ that charges $80/hour for someone who barely speaks Swahili and has no medical training. You think the interpreter who does your mother’s dialysis instructions is certified? Or are they a college student paid $15 an hour to wing it?
And don’t get me started on ‘culturally adapted labels.’ That’s just corporate jargon for ‘we’re too lazy to hire actual pharmacists who speak your language.’
This isn’t about access. It’s about control. The system wants you dependent - not informed.
Frank Geurts
January 18, 2026 AT 07:03Allow me to underscore, with the utmost gravity, that the provision of professional medical interpretation is not merely a courtesy - it is a non-negotiable ethical imperative, codified under Title VI of the Civil Rights Act of 1964, and reinforced by the Joint Commission’s National Patient Safety Goals. To neglect this duty is not merely a procedural lapse; it constitutes a fundamental violation of human dignity and the Hippocratic Oath.
Furthermore, the assertion that ‘family members can suffice’ is not only empirically unsound - it is dangerously negligent. Research from the Institute of Medicine (2004) and subsequent meta-analyses published in JAMA Internal Medicine (2019) confirm unequivocally that untrained interpreters introduce clinically significant errors in 22–37% of cases - errors that manifest as adverse drug events, hospital readmissions, and, in extremis, mortality.
The solution is not incremental. It is systemic. We must mandate certification, fund real-time video interpretation in every clinical setting, and integrate language preference into the EHR at the point of registration - not as an afterthought, but as a foundational pillar of care.
Let us not mistake compassion for compliance. We are not doing enough. We must do better - and we must do it now.
Amy Ehinger
January 18, 2026 AT 14:12I used to work at a pharmacy in Ohio, and we had this one elderly woman who spoke only Vietnamese. Her son always came with her - he was sweet, always smiling, but he’d just nod along when the pharmacist explained things. One day, I asked if she’d ever been given the label in Vietnamese. She just looked at me like I’d asked if she believed in aliens. Then she pulled out this folded-up piece of paper from her purse - it was a handwritten note from her daughter in California, translated line by line, with little drawings of pills and clocks. She didn’t need an interpreter. She needed someone to listen.
After that, we started printing simple pictograms on labels - a sun for morning, a moon for night, a red X for ‘don’t crush.’ No fancy tech. Just clarity. She stopped coming in with panic in her eyes.
Maybe the answer isn’t more interpreters. Maybe it’s just more care.
Nilesh Khedekar
January 19, 2026 AT 18:42Oh, here we go again - the ‘professional interpreter’ fairy tale. You really think a 22-year-old in a call center in Bangalore, paid $10/hour, knows the difference between ‘sublingual’ and ‘intramuscular’? Or that they care? The system is rigged. They don’t want you to understand - they want you to shut up and take the pill.
And don’t even get me started on ‘teach-back.’ That’s just a way for nurses to feel good about themselves while you’re still confused. ‘Can you explain this back?’ What if you’re scared? What if you’re ashamed? What if you think they’ll laugh at you?
Real solution? Train the damn pharmacists to speak Spanish, Mandarin, Tagalog - not hire a third-party vendor that outsources to a country where they can’t even pronounce ‘hypertension.’
And yes - I’ve been there. My dad took his blood thinner wrong because the ‘interpreter’ said ‘once a day’ was ‘every other day.’ He almost died. The hospital apologized. Then they sent him another prescription - in English.
RUTH DE OLIVEIRA ALVES
January 19, 2026 AT 22:56The structural inequities embedded within healthcare communication protocols are not incidental; they are systemic. The absence of linguistically appropriate materials constitutes a form of institutionalized discrimination, violating both statutory mandates and the ethical tenets of medical professionalism. The normalization of familial interpretation as an acceptable substitute reflects a profound epistemic injustice - the dismissal of non-English-speaking populations as inherently less capable of autonomous comprehension.
It is imperative that institutions implement mandatory, accredited interpreter certification programs, and that electronic health records be engineered to dynamically generate multilingual, culturally congruent pharmaceutical instructions - not as an add-on, but as a core function of patient safety infrastructure.
The FDA’s forthcoming labeling regulations represent a necessary, albeit insufficient, step forward. However, true equity demands more than policy amendments - it requires a paradigmatic shift in how we conceptualize language as a determinant of health.
Until language access is treated with the same urgency as sterile technique or medication reconciliation, we are not providing care - we are administering risk.
Ayush Pareek
January 21, 2026 AT 17:43I’ve seen this in my own village back in India - elders taking medicine wrong because the label was in English. We didn’t have interpreters. So we made pictures. We drew pills with arrows. We used colors. One old man didn’t know what ‘once daily’ meant - so we tied a red string around his wrist every morning. He lived to 92.
You don’t need fancy tech. You need someone who cares enough to slow down. To draw. To repeat. To sit with them.
Start small. Be the person who asks, ‘Do you need help reading this?’ That’s all it takes.
Iona Jane
January 22, 2026 AT 17:09They’re lying. All of them. The ‘certified interpreters’? Paid by the same hospitals that cut corners on everything else. The ‘FDA rules’? Just PR to distract from the fact that 90% of pharmacies still print labels in English only. And ‘teach-back’? That’s not safety - it’s a trap. They want you to admit you don’t understand so they can blame you when you die.
This isn’t about language. It’s about who gets to live - and who gets to be forgotten.