When OTC Diarrhea Medicines Help - and When They Can Hurt
Diarrhea hits fast. One minute you’re fine, the next you’re racing to the bathroom. It’s uncomfortable, embarrassing, and exhausting. Most of the time, it goes away on its own in a day or two. But that doesn’t mean you have to suffer. Over-the-counter (OTC) treatments like Imodium and Pepto-Bismol can give you relief - fast. But they’re not magic pills. Using them wrong can make things worse. Knowing when to reach for the bottle and when to call your doctor could mean the difference between a quick fix and a serious problem.
What’s Actually in These Pills?
Not all OTC diarrhea meds work the same way. There are two main types you’ll find on the shelf: loperamide and bismuth subsalicylate.
Loperamide (sold as Imodium, Diar-Aid, or store brands) slows down your gut. It’s a synthetic opioid, but don’t let that scare you - at normal doses, it doesn’t affect your brain. It works right in your intestines, reducing how fast food moves through. That means fewer trips to the bathroom. Studies show it cuts stool frequency by 40-62% within 24 hours. It starts working in 30 to 60 minutes. Most adults take 4 mg after the first loose stool, then 2 mg after each next one - but never more than 8 mg in a day.
Bismuth subsalicylate (Pepto-Bismol, Kaopectate) does more than just slow things down. It coats your stomach lining, soaks up toxins, reduces inflammation, and even kills some bacteria like E. coli and Campylobacter. It’s the only OTC option that helps with nausea and cramps too. You’ll see a 48% drop in stool frequency, but you’ll also notice something strange: your stool turns black. So does your tongue. That’s normal. It’s not bleeding - it’s just bismuth. It’s harmless, but it can freak you out if you don’t know why it’s happening.
Which One Should You Pick?
It depends on what’s bothering you.
If you’re just dealing with watery stools and no other symptoms - think food poisoning or a virus - loperamide is faster and more focused. You want to stop the diarrhea? Go with Imodium.
If you’ve got diarrhea plus nausea, stomach cramps, or you’re traveling to a place with sketchy water, bismuth subsalicylate is the better pick. It doesn’t just mask the problem - it fights it. And if you’re worried about traveler’s diarrhea, taking it before you eat or drink risky stuff can cut your risk by 65%.
But here’s the catch: you can’t take both together. Pepto-Bismol contains salicylates (similar to aspirin). Mixing it with other NSAIDs or taking too much can lead to serious toxicity. And loperamide? Don’t combine it with other anti-diarrheals. It’s not stronger - it’s riskier.

When You Shouldn’t Use Them at All
These meds are not for everyone. And they’re not for every kind of diarrhea.
If you have a fever over 100.4°F (38°C), you shouldn’t take either. Fever means your body is fighting an infection - maybe something like Salmonella or Shigella. Slowing your gut down traps those bugs inside. That can turn a bad case into a dangerous one. The same goes for bloody or black stools. That’s not just diarrhea - that’s a sign of inflammation, ulceration, or worse. Don’t mask it. Get checked.
Also skip these if you have severe abdominal pain. Diarrhea with cramping that doesn’t let up? Could be appendicitis, diverticulitis, or an intestinal blockage. OTC meds won’t fix that. They’ll just hide it until it’s too late.
And don’t give loperamide to kids under 12 without a doctor’s OK. The FDA has logged over 120 cases of serious side effects in children since 2010, including paralytic ileus - where the gut just stops working. Pepto-Bismol isn’t safe for kids under 12 either, thanks to the salicylate risk.
How Long Is Too Long?
Most cases of acute diarrhea last 1 to 3 days. If it’s still going after 48 hours, it’s time to stop the OTC meds and call your doctor.
Here’s what the experts say: if you’ve had more than six loose stools in 48 hours, or you’re showing signs of dehydration - dry mouth, dizziness, little or no urine, sunken eyes - you need medical care. Weight loss over 5% of your body weight in a few days? That’s a red flag too.
Even if you feel okay, persistent diarrhea can mean something deeper: a parasite like Giardia, a bacterial infection, or even something like Crohn’s disease. OTC meds don’t treat the cause. They just cover it up. And if you’re covering up a real problem, it can get worse.
The Real Danger: Taking Too Much
Here’s the scary part: people are abusing loperamide.
It’s cheap. It’s easy to get. And some people use it to manage opioid withdrawal symptoms - taking 50, 100, even 200 mg a day. That’s not treating diarrhea. That’s self-medicating for addiction. And it’s killing people.
The FDA has linked over 40 deaths between 1976 and 2015 to loperamide overdose. At high doses, it messes with your heart rhythm. It can cause QT prolongation - a dangerous arrhythmia that leads to cardiac arrest. You won’t feel it coming. One day you’re fine. The next, you’re in the ER.
Even without abuse, people accidentally overdose. They think, “I didn’t feel anything after one pill, so I’ll take two.” Or they keep taking it because they’re still having loose stools. But more isn’t better. It’s dangerous. The maximum safe dose is 8 mg in 24 hours - no exceptions.
What to Do Instead
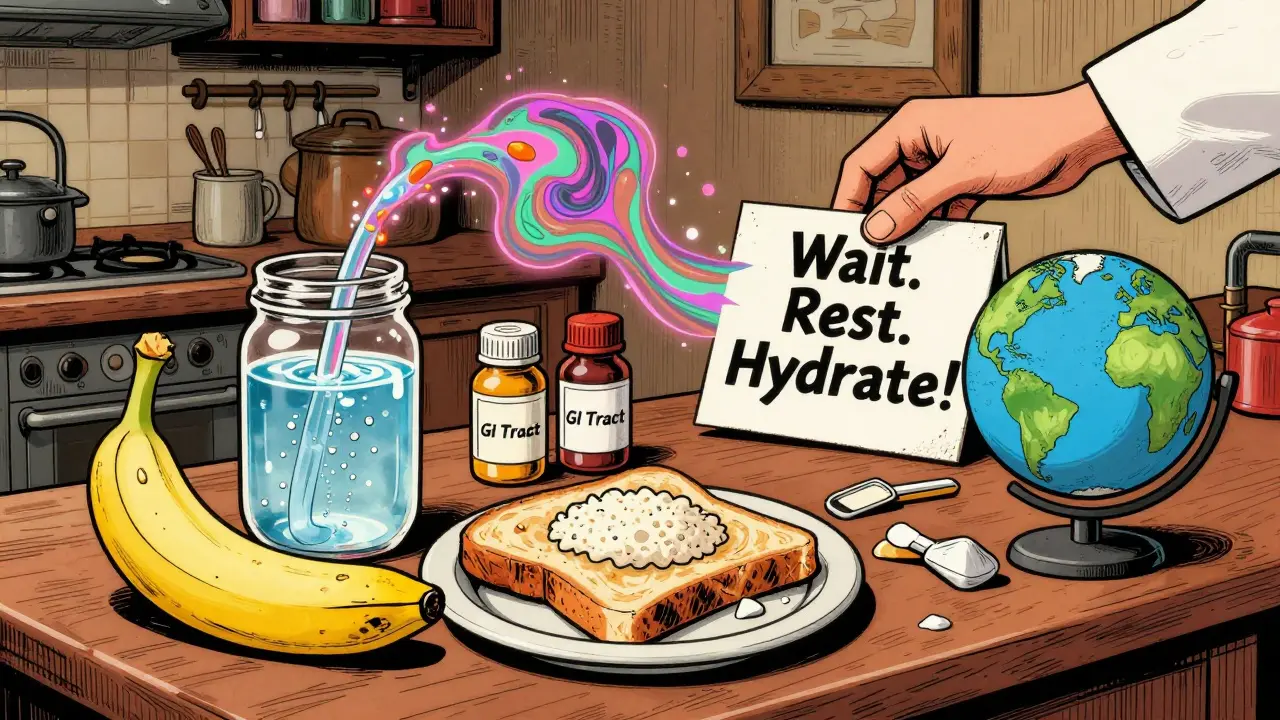
OTC meds aren’t the whole answer. Hydration is.
When you have diarrhea, you lose fluids and electrolytes. Water alone isn’t enough. You need something with sodium and glucose - like oral rehydration solutions (ORS). WHO-recommended ORS has 75 mmol/L of sodium. You can buy packets (like Pedialyte or generic brands) or make your own: 1 liter of clean water, 6 teaspoons of sugar, and half a teaspoon of salt.
Don’t drink soda, coffee, or alcohol. They make dehydration worse. Avoid dairy - your gut can’t digest lactose during diarrhea. Stick to the BRAT diet: bananas, rice, applesauce, toast. Simple, bland, easy to digest. Most pediatricians still recommend it.
Rest. Give your body time to heal. Don’t push through it. Diarrhea is your body’s way of flushing out something harmful. Fighting it with meds isn’t always the right move.
What’s New and What’s Changing
The market for OTC diarrhea meds is huge - over $1.2 billion in the U.S. alone. Imodium holds 58% of the share. Pepto-Bismol has 32%. But things are shifting.
The FDA now requires loperamide packaging to say “Do not exceed 8 mg per day.” That’s because of over 170 reported cardiac events between 2011 and 2019. Europe is even stricter - only 4 mg per day without a prescription.
Doctors are also changing their advice. The American College of Emergency Physicians now says: don’t routinely give anti-diarrheals in the ER. Focus on rehydration first. Antibiotics? Only if a specific bacteria is confirmed. Most cases are viral and don’t need them.
Future treatments might include racecadotril - a newer drug approved in Europe and Canada that reduces diarrhea duration by 24 hours in kids. But it’s not available OTC in the U.S. yet.
And with rising antibiotic resistance - 38% of traveler’s diarrhea cases now resist common drugs - OTC symptom control might become even more common. But that doesn’t mean it’s always the best choice.
Bottom Line: Know Your Limits
OTC diarrhea treatments are useful tools - but only when used correctly. They’re not for fever, blood in stool, severe pain, or long-lasting symptoms. They’re not for kids under 12 without a doctor’s approval. And they’re absolutely not for taking more than the label says.
If you’re unsure, wait. Drink water. Rest. Watch for warning signs. If it doesn’t improve in 48 hours - or if you feel worse - see a doctor. Diarrhea is usually harmless. But sometimes, it’s the first sign of something serious. Don’t let a quick fix delay the care you need.
Can I take Imodium and Pepto-Bismol together?
No. Pepto-Bismol contains salicylates (similar to aspirin), and combining it with other medications can increase the risk of toxicity. Imodium and Pepto-Bismol work differently, but taking both doesn’t make you better - it just raises your risk of side effects. Stick to one at a time.
Why does Pepto-Bismol turn my stool black?
The bismuth in Pepto-Bismol reacts with sulfur in your digestive tract, creating bismuth sulfide - a harmless black compound. It’s very common (98% of users see it) and goes away once you stop taking it. It’s not blood. But if you’re unsure, or if your stool is tarry and foul-smelling, check with a doctor to rule out bleeding.
Is loperamide safe for long-term use?
No. Loperamide is only meant for short-term, acute diarrhea. Using it daily for weeks or months can lead to dependence, severe constipation, or even heart rhythm problems. If you have chronic diarrhea, you need to find the root cause - not mask it. Talk to a doctor about tests for infections, IBS, Crohn’s, or other conditions.
Can I give Imodium to my 8-year-old?
Only under a doctor’s supervision. The FDA has approved Imodium liquid for children 6 and older, but only for specific cases. The risk of paralytic ileus - where the intestines stop moving - is real in kids. Never give caplets to children under 12. For kids, hydration and rest are safer than meds.
When should I go to the ER for diarrhea?
Go to the ER if you have: bloody or black stools, high fever (over 101.3°F), severe abdominal pain, signs of dehydration (no urine for 8+ hours, dizziness, rapid heartbeat), or if diarrhea lasts more than 48 hours without improvement. These aren’t normal - they’re warning signs that need urgent care.
Can OTC diarrhea meds prevent traveler’s diarrhea?
Bismuth subsalicylate (Pepto-Bismol) can reduce your risk by 65% if taken before meals and drinks in high-risk areas. Take two 262 mg tablets four times a day. But it’s not a guarantee. Avoid tap water, raw food, and undercooked meat. Hydration and food safety matter more than pills.

Phoebe McKenzie
January 1, 2026 AT 07:54Oh my god, people are STILL taking Imodium like it’s candy? 🤦♀️ I’ve seen so many friends turn into walking zombies because they thought ‘one more pill won’t hurt.’ Loperamide isn’t a chill pill-it’s a cardiac time bomb if you abuse it. And don’t even get me started on those ‘natural remedy’ TikTok influencers telling people to chug Pepto-Bismol like it’s a protein shake. Wake up, people. Your gut isn’t a magic box you can just slap a bandage on.
Stephen Gikuma
January 2, 2026 AT 06:24Big Pharma doesn’t want you to know this, but loperamide was originally developed by the government as a covert opioid suppressant. The 8mg limit? That’s a lie. They lowered it after the public started figuring out how to use it for withdrawal. Meanwhile, the FDA pushes Pedialyte like it’s holy water while ignoring the real solution: fasting and cold showers. America’s health system is broken-and this is just one symptom.
Bobby Collins
January 3, 2026 AT 13:47okay but why does pepto turn your tongue black?? i thought it was like… poison?? like is my body rotting?? also why do they not warn you on the bottle?? i thought i was dying for like 3 days lmao
LIZETH DE PACHECO
January 3, 2026 AT 16:31Thank you for writing this so clearly. I’ve had chronic diarrhea for years and was terrified to ask my doctor because I thought I was just ‘overreacting.’ This post gave me the courage to finally get tested-and turns out, I have SIBO. OTC meds were just hiding it. Hydration and probiotics changed my life. If you’re suffering long-term, please don’t suffer in silence. You deserve real answers.
Lee M
January 3, 2026 AT 17:30Diarrhea is nature’s way of saying you’ve been spiritually and physically contaminated. Loperamide doesn’t cure-it suppresses. You’re not healing. You’re avoiding the truth. The gut is the seat of the soul. When it rebels, it’s not about food. It’s about fear, guilt, and unresolved trauma. The real treatment? Silence. Stillness. And a 10-day water fast.
Dusty Weeks
January 4, 2026 AT 16:05bro i took 12 imodium once bc i was at a concert and didn’t wanna miss the set 🤡 it was bad. like… i couldn’t move. my stomach felt like concrete. i called my mom and she screamed at me for 20 mins. i still feel guilty. don’t be me.
Bill Medley
January 6, 2026 AT 08:06The information presented is accurate, evidence-based, and clinically responsible. The distinction between symptomatic relief and pathogen containment is critical. Public education on dosage limits and contraindications remains inadequate. This post serves as a necessary corrective.
gerard najera
January 8, 2026 AT 02:05We treat symptoms like enemies. But what if diarrhea is the body’s last honest messenger? We’ve forgotten how to listen. We reach for pills before we ask why. The real question isn’t ‘which drug?’ but ‘what is this trying to tell me?’
Heather Josey
January 10, 2026 AT 01:31This is such a vital resource. I’ve shared this with my entire family, especially my teenage nephew who thinks ‘a couple extra pills’ is fine. The part about cardiac risks shocked me-I had no idea. Thank you for emphasizing hydration over medication. We need more posts like this.
Olukayode Oguntulu
January 10, 2026 AT 08:24While your exposition on loperamide pharmacokinetics is technically competent, it remains epistemologically impoverished. You reduce a complex homeostatic response to a pharmacological binary: ‘good’ vs. ‘bad’ drug. The true pathology lies in the neoliberal commodification of bodily autonomy-where symptom suppression becomes a proxy for existential avoidance. Have you considered racecadotril’s ontological implications? No? Then your analysis is merely symptomatic.
jaspreet sandhu
January 10, 2026 AT 23:39Everyone in America takes medicine for everything. In India, we just drink buttermilk and rest. No pills. No panic. No drama. You people think diarrhea is a crisis. It’s just your body cleaning out bad food. You eat too much processed junk, then you blame the medicine for not fixing your bad habits. I’ve never taken Imodium in my life. Still alive. Still pooping. Still sane.
Alex Warden
January 12, 2026 AT 19:23Why is the FDA letting Chinese-made loperamide flood the market? I read that 70% of OTC meds in the U.S. are made in factories with no FDA oversight. That’s why people overdose. They’re getting fake pills with extra filler that messes with the heart. This isn’t medical negligence-it’s treason. We need to ban imports and make everything American-made. #BuyAmerican #StopThePoison
Austin Mac-Anabraba
January 13, 2026 AT 20:41Let’s analyze the cognitive dissonance here: the same population that demands ‘natural remedies’ and shuns pharmaceuticals is the same one that chugs Pepto-Bismol like it’s Gatorade. They trust a 1950s bismuth compound more than modern microbiome science. This isn’t health literacy-it’s tribalism dressed as pragmatism. The real crisis isn’t diarrhea. It’s the collapse of critical thinking.
Layla Anna
January 15, 2026 AT 01:16Bryan Anderson
January 17, 2026 AT 00:29Thank you for the clear, thoughtful breakdown. I’m a nurse and see patients every week who come in with loperamide toxicity. Most didn’t realize they were overdosing. Your point about hydration being more important than medication is spot-on. I always tell patients: ‘Drink something with salt and sugar before you reach for the pill.’ Simple, effective, and safe.