Palliative Care Symptom Management Calculator
This calculator helps determine appropriate opioid doses and monitoring schedules for palliative care patients based on symptom severity, type, and patient factors. All recommendations follow guidelines from NCHPC, NHS, and UPenn protocols.
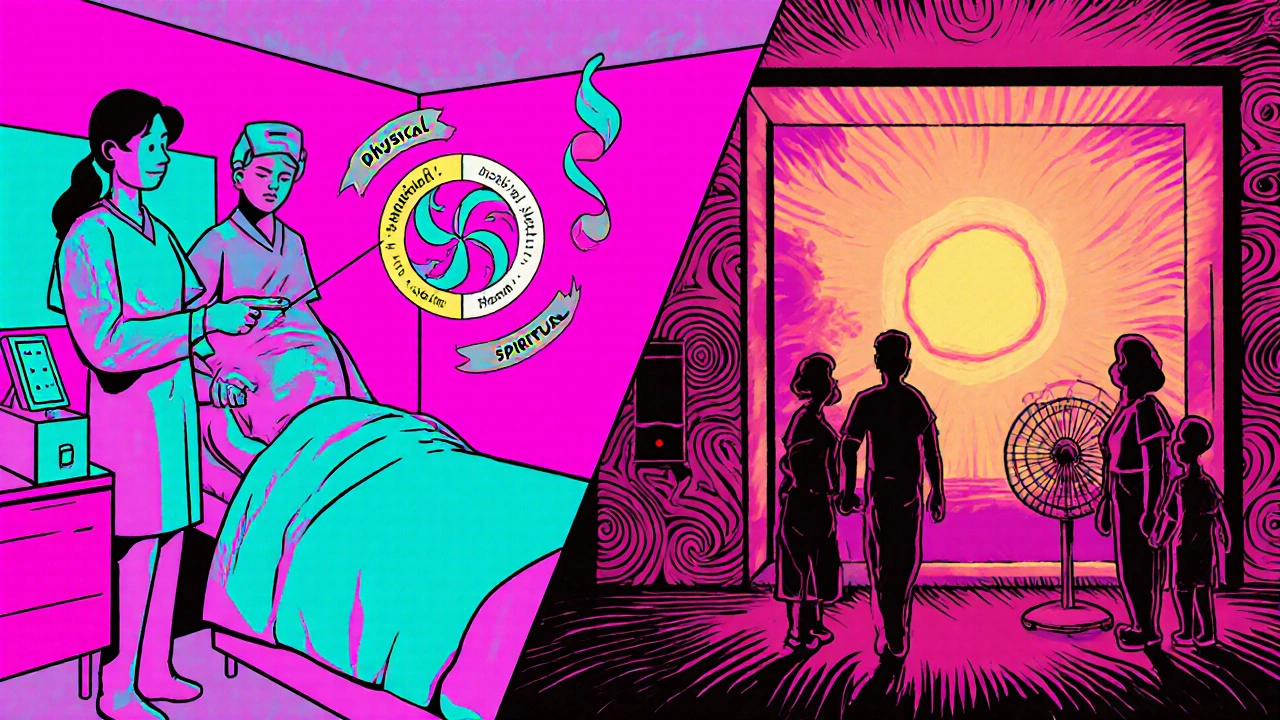
When a serious illness threatens quality of life, Palliative Care is specialized medical care that focuses on relieving physical, emotional, social, and spiritual suffering for patients and families. It isn’t limited to end‑of‑life moments; it can run alongside curative treatment from diagnosis onward. Hospice Care is a subset of palliative care for patients with a prognosis of six months or less who have chosen to stop disease‑directed therapy. The challenge clinicians face every day is how to control painful or distressing symptoms without adding a new layer of side effects that can erode the very comfort they’re trying to create.
Key Takeaways
- Use structured assessment tools (pain diagrams, numerical scales, CAM, RASS) to capture symptom intensity and trends.
- Start with low‑dose opioids for pain and dyspnea; titrate based on documented response every 30 minutes to an hour.
- Pair pharmacologic treatment with non‑drug strategies-positioning, fan therapy, mindfulness-to lower total medication load.
- Monitor for common side effects (sedation, constipation, delirium) and have rescue plans ready.
- Document every dose, timing, and assessment to meet CMS/MDS 3.0 requirements and reduce liability.
Understanding the Foundations
Two landmark documents shape today’s practice: the Clinical Practice Guidelines for Quality Palliative Care (4th ed., 2018) from the National Coalition for Hospice and Palliative Care (NCHPC) and the NHS North West Palliative Care Pain & Symptom Control Guidelines (2020). Both stress a holistic view-physical, psychological, social, and spiritual-yet they differ in how much detail they give to assessment forms. The NCHPC model breaks care into eight domains, making it easier to embed spiritual screening into routine visits. The NHS guide dives deep into pain description, using the “SOCRATES” mnemonic (Site, Onset, Character, Radiation, Associated factors, Time course, Exacerbating/relieving factors, Severity) and a body‑diagram to let patients point to multiple pain sites.
Core Symptom Domains and Assessment Tools
Effective symptom control starts with reliable data. Here are the three tools most clinicians rely on:
- Numerical Pain Scale (0‑10): Ask the patient to rate pain at rest, with movement, and after medication. Record the score in the electronic health record (EHR) every hour for the first 4 hours of a new opioid dose.
- Confusion Assessment Method (CAM) / CAM‑ICU: Use every 12 hours for patients at risk of delirium, especially after high‑dose opioids or anticholinergics.
- Richmond Agitation‑Sedation Scale (RASS): Check every 4 hours; a score of -4 to -5 signals oversedation and may require opioid taper.
When the assessment reveals dyspnea, the American Academy of Family Physicians (AAFP, 2017) rates opiates as a "B" level of evidence-effective and relatively safe when titrated slowly. For anxiety, UPenn Comfort Care Guidelines (2020) recommend lorazepam 0.5 mg PO/IV every 30 minutes PRN, but only after a documented anxiety score above 6 on a 0‑10 visual analog scale.
Medication Strategies and Side Effect Management
Below is a concise roadmap for the most common symptom clusters.
| Symptom | First‑line Drug | Typical Dose | Monitoring Interval |
|---|---|---|---|
| Pain (moderate‑severe) | Oxycodone | 5‑10 mg PO q4‑6h PRN | Every 30 min until stable, then q4h |
| Dyspnea | Morphine | 2‑4 mg PO q4h PRN | Every 30 min for first dose, then q4h |
| Delirium | Haloperidol | 1‑5 mg PO/IV q4‑6h PRN | CAM every 12h, RASS q4h |
| Anxiety | Lorazepam | 0.5 mg PO/IV q30 min PRN | Assess anxiety score q30 min |
| Excessive secretions | Hyoscyamine drops | 0.5 mg PO q6h PRN | Observe oral cobwebbing q2h |
Every drug comes with a side‑effect profile. Opioids can cause constipation, nausea, and respiratory depression. A simple bowel‑regimen-stool softener, stimulant laxative, and a low‑dose methylnaltrexone for opioid‑induced constipation-keeps the gut moving without cutting analgesia. For delirium, antipsychotics such as haloperidol require an ECG after the first 5 mg to watch QT prolongation; the UPenn protocols advise stopping the drug once the patient is comfortable and the CAM score is negative for at least 24 hours.
Balancing Non‑Pharmacologic Approaches
Guidelines agree that meds alone won’t solve everything. The NCHPC domains explicitly call for “psychosocial and spiritual assessment” in every visit. Here are three low‑cost interventions that cut medication needs by 15‑30 % in practice:
- Positioning and fan therapy: Elevating the head of the bed 30° and using a bedside fan reduces dyspnea scores without extra drugs.
- Mindfulness breathing: A 5‑minute guided session drops anxiety VAS scores by ~2 points (study, JAMA Internal Med, 2022).
- Family presence and narrative therapy: When families are invited to share the patient’s life story, existential distress falls, and opioid requirements dip according to Dr. Harvey Chochinov’s research.
Implementing Protocols in Clinical Settings
Rolling out a symptom‑control pathway takes coordination. The typical learning curve is 6‑12 months of supervised practice (NCHPC, 2018). A practical checklist helps teams stay on track:
- Assign a “symptom champion” - usually a nurse practitioner trained in the CAM, RASS, and pain‑diagram tools.
- Integrate the numerical pain scale into vitals intake; make it a required field in the EHR.
- Set automated alerts for opioid doses exceeding 30 mg oral morphine equivalents in 24 hours.
- Schedule a daily interdisciplinary huddle (physician, nurse, social worker, chaplain) to review assessment scores and adjust meds.
- Document every dose, timing, and patient‑reported effect; this satisfies CMS’s MDS 3.0 audit requirements and protects against reimbursement penalties.
Tele‑palliative care, now expanding to 40 % of rural patients (CAPC, 2023), can run the same assessments via video‑based pain diagrams and remote CAM administration, keeping care equitable.
Common Pitfalls and Pro Tips
Even seasoned clinicians stumble. Here are the most frequent mistakes and quick fixes:
- Skipping the pain‑type documentation: The NHS guideline shows that “many palliative patients have more than one pain.” Use separate entries for nociceptive, neuropathic, and breakthrough pain to avoid over‑medicating one pathway.
- Over‑sedation due to continuous opioid infusion: Follow the UPenn protocol of “assessment every 30 minutes while establishing comfort.” If RASS hits -4, pause the infusion and reassess.
- Ignoring constipation until it becomes severe: Start bowel regimen at opioid initiation, not after the first complaint.
- Family resistance to “strong” meds: Apply the NCHPC communication script: explain the right to live and die free of pain, provide visual analog scales to show expected benefit.
- Documentation fatigue: Use pre‑populated order‑sets that auto‑fill assessment timestamps; the 2008 Palliative Medicine study showed a 37 % rise in comfort scores when order‑sets were in place.
Future Directions: Precision Symptom Management
Research is moving toward genetics‑guided opioid dosing. A 2022 JAMA Internal Medicine study linked specific SNPs to 63 % of opioid‑response variability, hinting that a simple saliva test could soon inform the starting morphine equivalent. Meanwhile, digital symptom trackers-smartphone apps that feed real‑time VAS scores into the EHR-have improved control by 18 % in pilot programs (NCHPC, 2025). As these tools mature, the balance between control and side effects will shift from “trial‑and‑error” to “data‑driven personalization.”
Frequently Asked Questions
When should hospice care be introduced?
Hospice is appropriate once a patient’s life expectancy is six months or less and they decide to stop disease‑directed therapy. However, palliative services can start at diagnosis, and many clinicians transition the same team to hospice when the prognosis changes.
How often should I reassess pain after starting an opioid?
Check pain scores every 30 minutes for the first two doses. Once the score stabilizes (<2‑point change), move to every 4 hours unless breakthrough pain occurs.
What are the first‑line meds for delirium and their monitoring?
Haloperidol 1‑5 mg PO/IV PRN is the go‑to choice. Perform a baseline ECG, repeat if cumulative dose exceeds 10 mg, and run CAM every 12 hours plus RASS every 4 hours.
Can non‑pharmacologic measures replace opioids for dyspnea?
They can reduce opioid requirements but rarely eliminate the need entirely. Fan therapy, positioning, and short‑acting benzodiazepines together cut opioid dose by about 20 % in most studies.
What documentation is required for CMS compliance?
CMS mandates completion of the MDS 3.0 assessment, including pain, mood, and functional status, at admission and every 30 days. Missing fields can trigger 5‑15 % reimbursement penalties.
Jacqui Bryant
October 26, 2025 AT 12:44Great rundown on the basics-start low and titrate quickly, that’s the sweet spot. Using a pain diagram early on saves a lot of guesswork later. Don’t forget to pair meds with fan therapy; it really cuts down on dyspnea. Keep the bowel regimen going from day one, it prevents a cascade of problems.
Paul Luxford
November 9, 2025 AT 00:44Document every dose meticulously to stay audit‑ready.
Nic Floyd
November 22, 2025 AT 12:44The integration of multimodal assessment tools creates a feedback loop that optimizes analgesic titration 🚀 the Numerical Pain Scale provides a quantifiable baseline while the CAM and RASS add neurocognitive context 🧠 using these metrics in tandem supports a data‑driven approach that reduces reliance on subjective judgment 📊 the hourly documentation protocol for new opioid doses ensures pharmacokinetic steady‑state is achieved before escalation 🕒 it also allows rapid detection of over‑sedation, prompting timely dose adjustment 🛑 coupling low‑dose opioids with positioning strategies like 30‑degree head elevation can mitigate dyspnea without additional medication 🛏️ fan therapy, as highlighted, leverages thermoregulatory pathways to improve breathing comfort 🌬️ mindfulness breathing reduces anxiety VAS scores, thereby potentially lowering benzodiazepine use 🧘♂️ the bowel regimen, when initiated prophylactically, curtails opioid‑induced constipation before it becomes clinically significant 💊 incorporating stimulant laxatives early on maintains gut motility without compromising analgesia 🏃♀️ the use of methylnaltrexone in refractory cases offers peripheral opioid antagonism while preserving central pain control 🛡️ monitoring QT intervals after haloperidol initiation safeguards against arrhythmias, a critical safety net 📈 the interdisciplinary huddle model fosters real‑time communication among physicians, nurses, social workers, and chaplains, aligning goals of care 🤝 the digital symptom tracker apps feed real‑time VAS data into the EHR, enhancing responsiveness 📱 the genetic SNP testing on the horizon promises personalized opioid dosing, reducing trial‑and‑error cycles 🧬 the protocol’s emphasis on documentation fulfills CMS MDS 3.0 requirements, protecting against reimbursement penalties 📄 overall, this systematic, evidence‑based framework elevates patient comfort while minimizing iatrogenic side effects.
Johnae Council
December 6, 2025 AT 00:44Looks like someone took a school project and turned it into a corporate PowerPoint. All this talk about checklists and alerts, but where’s the human touch? Over‑reliance on numbers can make clinicians forget they’re dealing with real people. The “pro‑protocol” vibe feels more about liability than comfort.
Manoj Kumar
December 19, 2025 AT 12:44Ah, the noble quest to balance pain relief with side‑effects-like juggling flaming torches while blindfolded, isn’t it? Yet the guidelines promise a tidy roadmap, as if every patient fits a single template. Sure, low‑dose opioids are the starter pistol, but the marathon of hospice care is never that linear. One could argue that the emphasis on metrics masks the messy reality of existential suffering. Still, I’ll toast to the pragmatic wisdom of fan therapy; it’s the cheap miracle we all need. And let’s not forget that every algorithm is written by someone who probably never held a dying hand.
Hershel Lilly
January 2, 2026 AT 00:44It’s fascinating how the integration of remote video pain diagrams can expand access for rural patients while preserving assessment fidelity.
Carla Smalls
January 15, 2026 AT 12:44Love the reminder that a simple family story session can lower opioid needs-small gestures truly make a big difference. Keep the optimism flowing, teams!
Monika Pardon
January 29, 2026 AT 00:44Indeed, one might wonder whether the proliferation of checklists is a covert attempt to outsource clinical judgment to bureaucratic algorithms; however, the formal language herein clearly reflects an earnest commitment to patient-centered care, albeit couched in a veneer of procedural rigidity.
Rhea Lesandra
February 11, 2026 AT 12:44Team, remember that each assessment tool is a conversation starter, not a verdict. By inviting patients to describe their pain using the SOCRATES framework, you empower them to shape their own care plan. Likewise, integrating spiritual screening as a routine part of the visit normalizes reflection on meaning and purpose. This inclusive approach builds trust and often reveals hidden sources of distress that medication alone cannot address.
Kasey Marshall
February 25, 2026 AT 00:44Minimalist note: daily huddles keep everyone aligned and reduce duplicated work.