Smoking Medication Risk Calculator
Input Your Details
Risk Assessment Results
When you smoke, your body doesn’t just absorb nicotine-it changes how your liver processes medications. This isn’t theory. It’s a well-documented, clinically significant shift that affects hundreds of thousands of people every year. If you’re on medication and you smoke-or you recently quit-you could be at risk for treatment failure, dangerous side effects, or unexpected hospital visits. The culprit? A group of liver enzymes turned up to maximum by chemicals in cigarette smoke.
What Happens in Your Liver When You Smoke
Tobacco smoke doesn’t just harm your lungs. It floods your bloodstream with polycyclic aromatic hydrocarbons (PAHs), chemicals that trigger a chain reaction in your liver. These compounds bind to a receptor called the aryl hydrocarbon receptor (AhR). Once activated, this receptor tells your liver cells to produce more of certain drug-metabolizing enzymes, especially CYP1A2, CYP1A1, and CYP2E1. Think of these enzymes like tiny scissors that chop up medications so your body can get rid of them. When smoking increases their numbers, those scissors start cutting faster.Studies show that smokers have up to 40% more CYP1A2 activity than non-smokers. That means drugs processed by this enzyme get cleared from your body much quicker. The result? Lower drug levels in your blood. If you’re taking a medication that needs to stay at a certain concentration to work-like theophylline for asthma or clozapine for schizophrenia-your dose might be too low. You might feel like the drug isn’t working, when in reality, your body is just burning it off too fast.
Enzyme induction doesn’t happen overnight. It takes about 10 to 14 days of regular smoking for this effect to fully develop. But here’s the twist: when you quit, the process reverses. Within 72 hours, enzyme activity starts dropping. By two to four weeks after your last cigarette, your liver is back to normal. If your medication dose hasn’t been adjusted, you could suddenly have too much drug in your system. That’s when toxicity kicks in.
Medications Most Affected by Smoking
Not all drugs are affected equally. The big winners-meaning the ones most impacted-are those primarily broken down by CYP1A2. Here’s what the data shows:- Theophylline: Used for asthma and COPD. Smokers clear it 58-100% faster. Half-life drops from 8 hours to just 3 hours. Many patients on this drug require doses 50% higher than non-smokers. When they quit, levels can spike dangerously-leading to seizures, heart arrhythmias, or even death.
- Clozapine: An antipsychotic for treatment-resistant schizophrenia. Smokers need 50% more of this drug to reach the same blood levels as non-smokers. A 2023 FDA review found 147 cases of clozapine toxicity linked to smoking cessation, with 89% occurring within two weeks of quitting.
- Olanzapine: Another antipsychotic. Smokers have 98% higher clearance. Their blood levels drop by 12%. Dose adjustments are often needed.
- Duloxetine: An antidepressant and pain medication. Smokers metabolize it 30% faster. This can lead to reduced effectiveness, especially in chronic pain or depression.
- Caffeine: Yes, caffeine. It’s a common test drug for CYP1A2 activity. Smokers clear caffeine 30-50% faster. That’s why many smokers say they need more coffee to feel awake.
- Methadone: Used for opioid addiction. Smoking increases its clearance by about 15%, which can lead to withdrawal symptoms if doses aren’t adjusted.
- Mexiletine: A heart rhythm drug. Smokers have 36% shorter half-lives. This increases risk of arrhythmias if not monitored.
Drugs like SSRIs (e.g., sertraline, fluoxetine) and beta-blockers like propranolol are also affected, but less predictably. Propranolol levels drop 25% in smokers, which can reduce its heart-protective effects. The American Society of Health-System Pharmacists now recommends checking smoking status before prescribing any of these drugs.
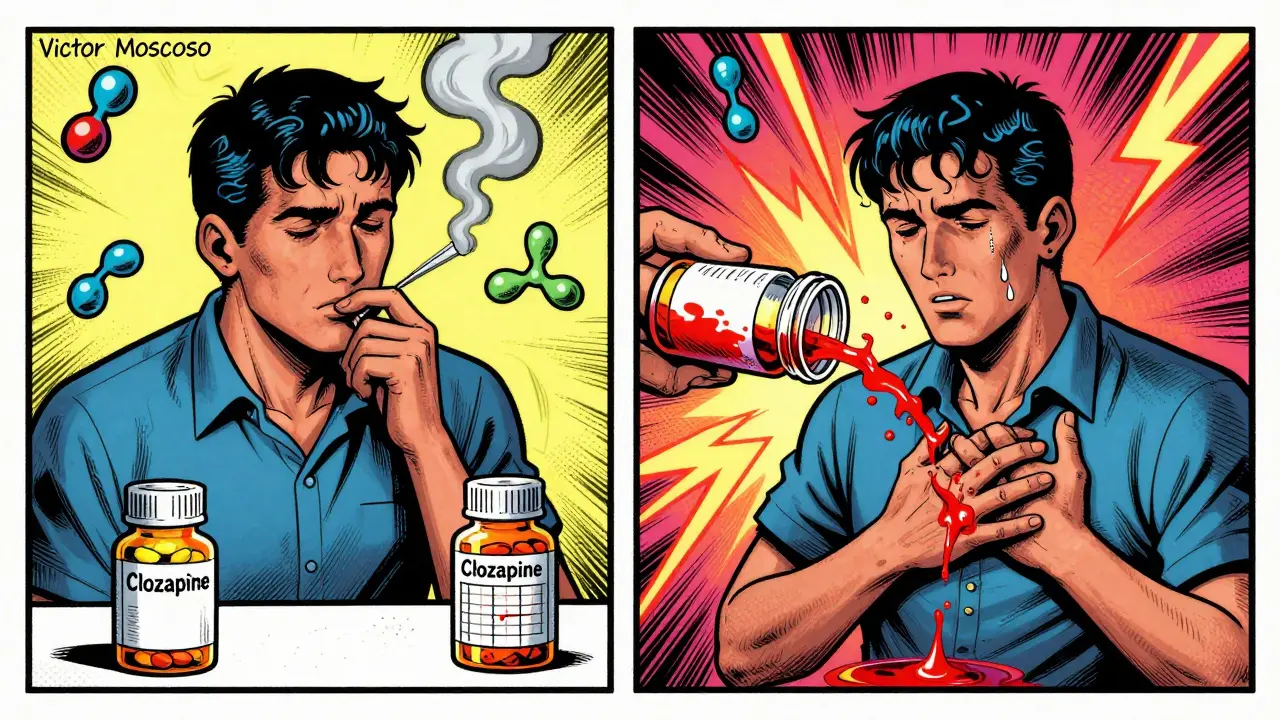
The Hidden Danger: Quitting Smoking
Most people think the risk ends when they smoke. But the real danger often comes after quitting. Patients who stop smoking without telling their doctor are walking into a trap. Their medication dose, which was fine while smoking, suddenly becomes too high. Enzyme levels drop, but the drug dose doesn’t. Blood concentrations rise. And that’s when problems start.Pharmacists report cases weekly. One Reddit user, u/Pharmacist_Jane, shared: “Had a patient hospitalized for theophylline toxicity 10 days after quitting smoking-levels went from subtherapeutic to toxic without dose change.” Another patient on DiabetesDaily.com wrote: “My A1C dropped from 7.8% to 5.9% two weeks after quitting smoking. I didn’t change my meds. My doctor didn’t warn me.” That’s pioglitazone, a diabetes drug, building up in her system because smoking had been speeding up its metabolism.
According to the UCSF Smoking Cessation Leadership Center, the highest risk window is days 3 to 14 after quitting. That’s when enzyme activity drops fastest, and drug levels rise fastest. Yet, fewer than 40% of primary care doctors routinely screen for smoking status when prescribing these medications. That’s a gap in care-and it’s dangerous.
What Clinicians Should Do
The solution isn’t complicated. It’s about awareness and protocol.- Ask every patient: “Do you smoke? How many cigarettes a day?” Document it. Not just once-every visit.
- For new smokers: If someone starts smoking while on a CYP1A2-metabolized drug, monitor drug levels weekly. Increase dose by 20-50% as needed.
- For patients quitting: Reduce the dose of affected drugs by 25-50% within 3-7 days of cessation. Don’t wait for symptoms. Proactively adjust.
- Use tools: The UCSF Drug Interactions Table and the new SmokeMetrix® diagnostic test (FDA-approved in 2023) can help quantify enzyme activity through caffeine metabolism.
- Update EHRs: Hospitals that added smoking status as a mandatory field in electronic records saw a 42% drop in related adverse events.
The American Pharmacists Association calls this “the most common preventable cause of medication-related hospitalizations among smokers.” The annual cost to the U.S. healthcare system? Over $2.3 billion.
What You Should Do
If you smoke and take any of the medications listed above:- Don’t assume your dose is right. Talk to your pharmacist or doctor.
- If you’ve recently quit smoking, tell your prescriber immediately-even if you feel fine.
- If you’re thinking about quitting, ask: “Will this affect my meds?”
- Keep a list of your medications and share it with every provider.
- Use the CDC’s free Smoking Cessation and Medication Management toolkit-it’s updated quarterly and free to download.
If you’re a smoker and your medication seems less effective, it might not be your condition worsening. It might be your liver working overtime.
What’s Changing in 2026
The field is evolving fast. The FDA now requires all new drugs metabolized by CYP1A2 to include smoking interaction data on their labels. The WHO launched a global initiative in January 2023 to make smoking status a standard part of electronic health records by 2027. And researchers at UCSF are testing a smartphone app that uses your breath to estimate enzyme activity in real time-no blood test needed.One thing is clear: smoking isn’t just a lifestyle choice. It’s a drug interaction waiting to happen. Ignoring it doesn’t make it go away. It just makes your meds less safe.
Does smoking affect all medications?
No. Smoking mainly affects drugs metabolized by CYP1A2, CYP1A1, CYP2E1, and some UGT enzymes. Medications processed by CYP2D6 (like many SSRIs) or CYP3A4 (like statins) are mostly unaffected. But if you’re on theophylline, clozapine, olanzapine, duloxetine, or methadone, smoking definitely changes how your body handles them.
How long after quitting smoking do drug levels change?
Enzyme activity starts dropping within 72 hours. The biggest change happens between days 3 and 14 after quitting. That’s why doctors recommend reducing doses of affected medications during this window. Full reversal takes 2-4 weeks. Don’t wait for symptoms-act early.
Can I just stop smoking to improve my meds?
Quitting smoking is always a good idea-but not without talking to your doctor first. If you’re on a medication affected by CYP1A2, quitting can cause dangerous drug buildup. Your dose may need to be lowered. Don’t assume your meds will work better on their own. They might work too well-and that’s risky.
Is there a test to check if smoking is affecting my drug levels?
Yes. A new FDA-approved test called SmokeMetrix® measures how fast your body clears caffeine, which directly reflects CYP1A2 enzyme activity. It’s a simple saliva or blood test. It’s being used in clinics now to guide dosing for patients on clozapine, theophylline, and other affected drugs.
What should I do if I’m trying to quit smoking and I’m on medication?
Tell your doctor and pharmacist before you quit. Ask: “Which of my meds are affected by smoking?” Get a plan in place. You may need dose adjustments, blood tests, or follow-up visits. The CDC’s Smoking Cessation and Medication Management toolkit has free guides for patients and providers.
