Which SNRI Might Be Right For You?
This tool helps identify which SNRI might be most appropriate based on your symptoms and concerns. Remember: Only a doctor can prescribe medication. This is for informational purposes only.
1. What are your primary symptoms?
When you're struggling with depression or chronic pain, finding the right medication can feel like searching for a key in a dark room. SNRIs-serotonin-norepinephrine reuptake inhibitors-are one of the most common keys doctors hand out. Unlike older antidepressants that only target serotonin, SNRIs work on two neurotransmitters at once: serotonin and norepinephrine. That dual action makes them especially useful for people who have both low mood and physical pain, like nerve pain from diabetes or the constant aches of fibromyalgia.
What Are SNRIs and How Do They Work?
SNRIs don’t just boost serotonin like SSRIs do. They also block the reabsorption of norepinephrine, a chemical linked to alertness, energy, and pain control. This dual effect is why SNRIs are often chosen when someone has depression along with fatigue, lack of motivation, or unexplained body pain. The first SNRI approved by the FDA was venlafaxine (Effexor) in 1993. Since then, others like duloxetine (Cymbalta), desvenlafaxine (Pristiq), and levomilnacipran (Fetzima) have joined the list.
Each SNRI has a slightly different balance. For example, duloxetine and desvenlafaxine are more focused on serotonin, while levomilnacipran and milnacipran lean more toward norepinephrine. This matters because norepinephrine plays a bigger role in pain signals and energy levels. That’s why duloxetine is approved not just for depression but also for diabetic nerve pain, fibromyalgia, and chronic back pain-conditions where SSRIs often fall short.
These drugs don’t work like stimulants. They don’t give you an instant high. Instead, they slowly help your brain restore balance. Most people notice changes in mood or pain after 4 to 6 weeks. Some report feeling more awake or less overwhelmed by physical discomfort even before their sadness lifts.
Venlafaxine: The Original SNRI
Venlafaxine was the first SNRI on the market, and it’s still one of the most prescribed. It comes in extended-release form (Effexor XR) to reduce stomach upset and allow once-daily dosing. Starting doses are low-usually 37.5 mg per day-to help your body adjust. The typical therapeutic range is 75 to 225 mg daily, but higher doses (over 150 mg) come with a catch: increased blood pressure.
Studies show that about 12 to 15% of people taking venlafaxine at doses above 150 mg develop hypertension. That’s why doctors often check blood pressure regularly if you’re on a higher dose. It’s not dangerous for most, but it’s something you need to watch. People with existing high blood pressure or heart disease may be advised to avoid it.
Venlafaxine is also known for giving people more energy than SSRIs. Many users report feeling less sluggish, more motivated, and better able to get through the day. But that same energy boost can backfire-some people feel jittery or anxious at first. That usually fades within a couple of weeks.
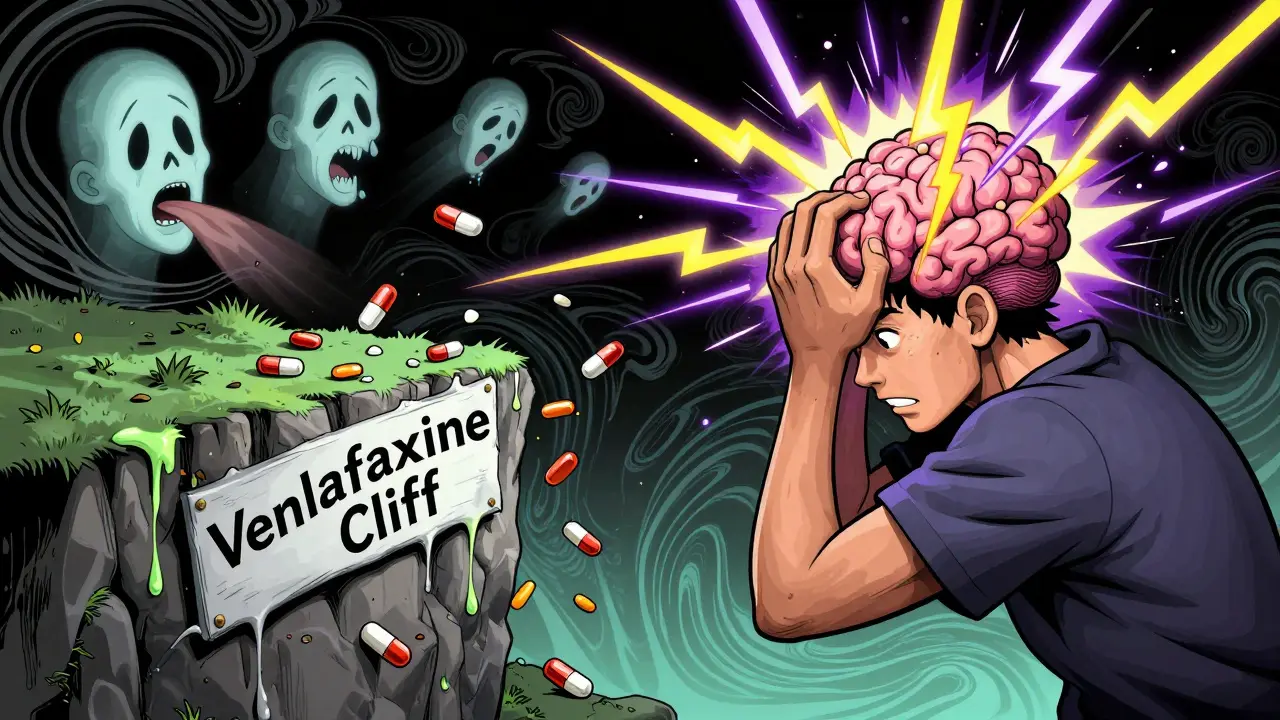
The biggest issue with venlafaxine? Withdrawal. If you stop suddenly, 50% or more of users experience what’s called discontinuation syndrome. Symptoms include dizziness, brain zaps (electric-shock-like feelings), nausea, irritability, and intense insomnia. The “venlafaxine cliff” is a real thing-missing even one dose can trigger symptoms. That’s why tapering slowly over 2 to 4 weeks is critical. Most doctors now recommend reducing the dose by 10 to 25% every week.
Duloxetine: The Pain and Mood Double Agent
Duloxetine (Cymbalta) stands out because it’s approved for more conditions than any other SNRI. It treats major depression, generalized anxiety disorder, diabetic nerve pain, fibromyalgia, and chronic musculoskeletal pain. That makes it a go-to for people whose depression and pain feed off each other.
Up to 30% of people starting duloxetine feel nauseous in the first week. For many, it gets better after 2 to 4 weeks. Taking it with food helps. Some users report initial weight loss-around 5 to 7 pounds in the first few months-likely from reduced appetite. But long-term use can lead to weight gain, which surprises some people.
Duloxetine is less likely than venlafaxine to raise blood pressure, making it a safer option for people with cardiovascular concerns. But it’s not gentle on the stomach. Dry mouth, constipation, and sweating are common. About 20% of users sweat more than usual, especially at night.
One of the most reported benefits? Pain relief. People with long-term back pain or nerve pain often say duloxetine gives them their first real sense of relief in years. For others, it’s the mood lift. But like all SNRIs, sexual side effects are common-about 65% of users report lower libido, delayed orgasm, or trouble reaching climax. That’s one of the hardest trade-offs.

Other SNRIs: What’s Different?
Desvenlafaxine (Pristiq) is essentially the active metabolite of venlafaxine. It’s marketed as having fewer drug interactions and a simpler dosing schedule. But in practice, its side effects and effectiveness are very similar. It’s not more powerful-just a different version of the same thing.
Levomilnacipran (Fetzima) is the most norepinephrine-focused SNRI. It’s often chosen when energy and focus are the main goals. Users report feeling more alert and mentally clear. But because it boosts norepinephrine so strongly, it can increase heart rate and blood pressure more than others. It’s not usually the first pick unless someone has tried other SNRIs without success.
Milnacipran (Savella) is approved only for fibromyalgia-not depression. It’s used in the U.S. mostly for that one condition. It’s not as widely prescribed as venlafaxine or duloxetine, but for fibromyalgia patients who haven’t responded to other treatments, it can be a game-changer.
Common Side Effects: What to Expect
Side effects vary from person to person, but some show up again and again:
- Nausea - Happens in 25-30% of users, especially with duloxetine. Usually fades in 2-4 weeks.
- Sexual problems - Affects 20-40% across all SNRIs. Lower desire, delayed orgasm, or inability to climax are most common.
- Dizziness and lightheadedness - Especially when standing up fast. Can be worse at the start of treatment.
- Increased sweating - Reported in 20% of duloxetine users, 15% of venlafaxine users.
- Constipation and dry mouth - Less severe than with older antidepressants, but still common.
- Insomnia or sleepiness - Some feel wired; others feel tired. Dosing time (morning vs. night) can help manage this.
More serious risks include serotonin syndrome-a rare but dangerous condition caused by too much serotonin in the brain. It’s most likely to happen if you mix SNRIs with other serotonergic drugs like tramadol, certain migraine meds (triptans), or St. John’s wort. Symptoms: confusion, rapid heart rate, high fever, muscle rigidity, seizures. If you experience these, seek help immediately.
SNRIs also increase bleeding risk because they reduce serotonin in platelets. That means you might bruise more easily or bleed longer after cuts or dental work. If you’re on blood thinners or have a bleeding disorder, talk to your doctor before starting.
How SNRIs Compare to Other Antidepressants
Compared to SSRIs like fluoxetine (Prozac) or sertraline (Zoloft), SNRIs have a broader effect. That’s why they’re often chosen for depression with fatigue, low energy, or physical pain. SSRIs are usually better for pure anxiety or OCD. SNRIs tend to be more activating, which can help people who feel stuck or numb.
Compared to older tricyclic antidepressants (TCAs), SNRIs are much safer. TCAs can cause dangerous heart rhythm changes, extreme dry mouth, constipation, and weight gain. SNRIs don’t have those risks. They’re also easier to tolerate long-term.
But they’re not perfect. SNRIs don’t work for everyone. About 30-40% of people don’t respond to the first antidepressant they try. That doesn’t mean you’re broken-it just means your brain needs a different approach. Some people switch to an SSRI, add a different medication, or try therapy alongside meds.
Real User Experiences
On patient forums, people describe venlafaxine as “the only thing that brought me back to life” and “the drug that ruined my sleep and made me feel like I was losing my mind.” Duloxetine gets similar split reviews: “It killed my pain” versus “I couldn’t have sex anymore and gained 15 pounds.”
One user wrote: “I was on Zoloft for a year. My pain didn’t change. I started duloxetine. Within three weeks, I could walk without screaming. But I stopped having orgasms. I chose the walking.”
Another said: “I missed one dose of venlafaxine. Felt like I was in a car crash. Brain zaps, nausea, panic. I cried for three days. I’ll never stop cold again.”
These stories aren’t outliers. They’re common. That’s why communication with your doctor matters more than the drug itself.
What You Need to Know Before Starting
- Start low, go slow. Most side effects are worst in the first 2 weeks. Don’t quit because you feel sick at first.
- Don’t stop suddenly. Taper over at least 2-4 weeks. Your doctor should give you a plan.
- Watch your blood pressure. Especially with venlafaxine over 150 mg/day. Check it at home if you can.
- Check for interactions. Avoid mixing with MAOIs, tramadol, or certain painkillers. Always tell your doctor what else you’re taking.
- Give it time. Mood and pain improvements take 4-8 weeks. Don’t judge it after 10 days.
- Sexual side effects are common. Talk to your doctor. There are strategies-dosage adjustments, timing changes, or adding medications like bupropion-that can help.
SNRIs aren’t magic pills. But for many people, they’re the best tool they’ve found to reclaim their life. If one doesn’t work, another might. And if none do, there are still other options-therapy, lifestyle changes, or newer treatments in development.
What’s Next for SNRIs?
Research is ongoing. Scientists are looking at how SNRIs affect inflammation in the brain, which might explain why they help with pain beyond just neurotransmitter changes. Newer versions are being tested to balance serotonin and norepinephrine more evenly, hoping to reduce side effects while keeping benefits.
As of 2025, over 40 clinical trials are exploring SNRIs for PTSD, ADHD, and menopausal hot flashes. The market is growing-not because they’re perfect, but because they work for people who didn’t respond to anything else.
SNRIs have helped millions. But they’re not for everyone. The key is knowing what you’re signing up for-and having a plan to manage the downsides.
Can SNRIs cause weight gain?
Yes, but it’s complicated. Many people lose a few pounds in the first few weeks due to reduced appetite, especially with duloxetine. But over time-after 6 to 12 months-some gain weight. This is likely due to improved mood leading to increased eating or metabolic changes. Weight gain isn’t as common or severe as with older antidepressants like amitriptyline, but it’s still a possibility.
Do SNRIs work faster than SSRIs?
Not necessarily for mood, but sometimes for energy and pain. Both types take 4-6 weeks to fully help depression. But SNRIs often improve fatigue and physical symptoms sooner because of their effect on norepinephrine. Some people report feeling more alert within 1-2 weeks, while SSRIs might take longer to lift that heaviness.
Are SNRIs addictive?
No, SNRIs are not addictive in the way drugs like opioids or benzodiazepines are. You won’t crave them or get high from them. But your body adapts to them. Stopping suddenly can cause withdrawal symptoms-dizziness, brain zaps, nausea, anxiety-which feel like addiction but are actually your nervous system readjusting. That’s why tapering is essential.
Can I drink alcohol while taking SNRIs?
It’s not recommended. Alcohol can worsen dizziness, drowsiness, and liver stress. It can also increase the risk of serotonin syndrome and make depression worse. Even moderate drinking can interfere with how well the medication works. If you drink, talk to your doctor about safe limits-or better yet, cut back while on treatment.
What if SNRIs don’t work for me?
You’re not alone. About 1 in 3 people don’t respond to the first antidepressant they try. If SNRIs don’t help after 8-12 weeks, your doctor might switch you to an SSRI, a different class like bupropion, or add a medication like lithium or thyroid hormone. Therapy, exercise, and sleep improvements can also make a big difference. Don’t give up-finding the right fit often takes time and patience.

Dave Alponvyr
December 15, 2025 AT 19:03SNRIs: because nothing says 'I'm better' like brain zaps and zero libido.
Tiffany Machelski
December 16, 2025 AT 11:42i started duloxetine last month and wow the brain zaps are real?? i missed a dose and felt like i got hit by a truck 😵💫
Kayleigh Campbell
December 17, 2025 AT 06:42My doctor called it 'the walking drug.' I traded orgasms for being able to carry groceries without crying. Worth it. 🤷♀️
Arun ana
December 18, 2025 AT 18:06Been on venlafaxine for 2 years. The energy boost saved my life, but the withdrawal? Bro, I had to taper over 10 weeks. One day I forgot and took a 37.5mg instead of 12.5 - woke up screaming. 😣
Also, the sweating? Like I’m in a sauna at 3am. My wife says I smell like a gym sock. But hey - I can get out of bed now. 🙏
SHAMSHEER SHAIKH
December 19, 2025 AT 16:34It is imperative to note, with the utmost gravity, that SNRIs are not a panacea - they are a tool, a carefully calibrated instrument in the arduous journey toward neurological equilibrium. One must approach their use with reverence, discipline, and rigorous monitoring of blood pressure, sexual function, and the terrifying phenomenon known as 'brain zaps' - which, I assure you, are not metaphorical.
Many patients, in their desperation, abandon treatment prematurely, unaware that the initial nausea and dizziness are but the whispers of the nervous system adjusting to its new rhythm. Patience, dear friends, is not optional - it is sacred.
Moreover, the societal stigma surrounding antidepressants is a cruel illusion. Depression is not weakness. Pain is not laziness. And SNRIs? They are not 'chemical crutches' - they are the scaffolding that allows the soul to rebuild.
I have witnessed patients rise from bedridden despair to walking their children to school. That is not magic. That is science. And it deserves respect.
Do not fear the taper. Do not silence your symptoms. Speak to your physician. Keep a journal. Track your sleep. Note your appetite. Your body is speaking - listen.
James Rayner
December 19, 2025 AT 17:23I used to think SNRIs were just 'stronger SSRIs'... until I realized they don’t just change how you feel - they change how you exist in your body.
It’s weird. You wake up and your back doesn’t scream. You walk downstairs and you don’t need to brace yourself. But then you realize you haven’t felt a kiss in six months.
Is that healing? Or just trading one kind of pain for another?
I don’t know. But I’m still here. And that’s something.
Josias Ariel Mahlangu
December 20, 2025 AT 11:59People complain about side effects like they’re entitled to a perfect life with zero trade-offs. You want to feel better? Then accept the cost. Life isn’t a Netflix show where you get to pick your side effects.
My cousin took venlafaxine, lost 15 pounds, and got her job back. She didn’t care that she couldn’t orgasm - she cared that she could get out of bed. Grow up.
Hadi Santoso
December 22, 2025 AT 05:31sooo i took duloxetine for fibro and yeah the sweat was wild like i was doing yoga in a sauna 😅
but also?? i finally played with my dog again after 3 years. he licked my face and i cried. so yeah. worth it.
also i typo a lot but i think u get the point lol
Billy Poling
December 23, 2025 AT 20:30It is incumbent upon the reader to understand that the efficacy of serotonin-norepinephrine reuptake inhibitors, while statistically significant in controlled clinical trials, is not universally reproducible in the heterogeneous population of individuals suffering from affective and somatic disorders. The reduction of depressive symptomatology, as measured by the Hamilton Depression Rating Scale, demonstrates a mean improvement of 42.3% over placebo, yet the incidence of adverse events - particularly gastrointestinal disturbance and sexual dysfunction - remains alarmingly high, with rates exceeding 65% in some cohorts. Furthermore, the phenomenon of discontinuation syndrome, often mischaracterized by laypersons as 'withdrawal' or 'addiction,' is in fact a neuroadaptive response to abrupt cessation of monoaminergic modulation, and must be managed with a structured, evidence-based tapering protocol extending over a minimum of fourteen days, though twenty-one to twenty-eight days is preferable. It is also noteworthy that the long-term metabolic consequences of SNRI use, particularly with regard to weight gain, remain inadequately studied in longitudinal analyses beyond twelve months. Therefore, clinicians must engage in shared decision-making, ensuring that patients are fully informed of both the therapeutic potential and the physiological trade-offs inherent in this pharmacological class.