St. John’s Wort might seem like a safe, natural fix for low mood. You’ve seen the bottles in the supplement aisle-cheap, easy to buy, no prescription needed. But here’s the truth most labels won’t tell you: St. John’s Wort doesn’t just treat depression. It can shut down the effectiveness of life-saving drugs you’re already taking.
How St. John’s Wort Changes How Your Body Handles Medication
St. John’s Wort isn’t just another herb. It’s a powerful enzyme inducer. That means it tells your liver to speed up the breakdown of certain drugs. The main culprit? Hyperforin. This compound activates something called the pregnane-X-receptor, which flips a switch in your body to produce more of the enzymes that metabolize medications.
These enzymes-CYP3A4, CYP2C9, CYP1A2-are the same ones that process about half of all prescription drugs. When St. John’s Wort cranks them up, your body clears those drugs too fast. The result? The medication doesn’t stay in your system long enough to work.
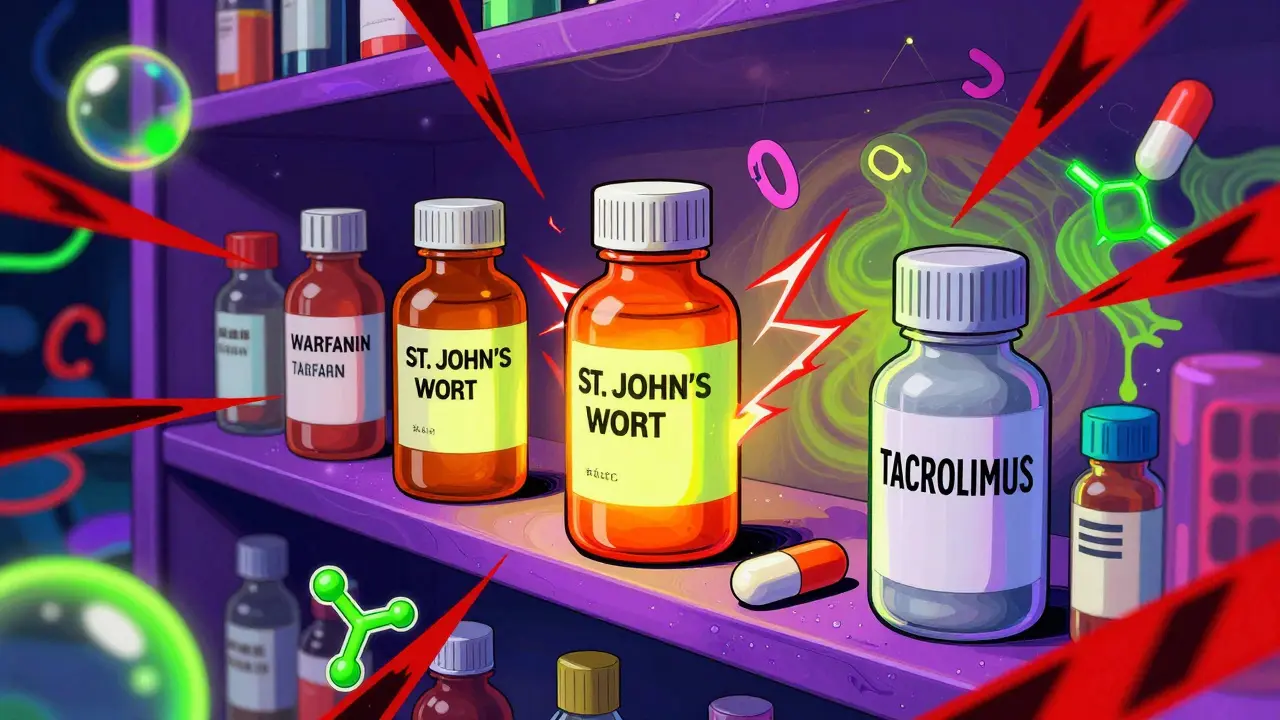
It’s not magic. It’s chemistry. And it’s not subtle. A 2019 case report described a kidney transplant patient whose tacrolimus levels dropped from a safe 12 ng/mL to 3 ng/mL within weeks of starting St. John’s Wort. Tacrolimus keeps the body from rejecting the new organ. That drop meant acute organ rejection. That’s not a side effect. That’s a medical emergency.
Medications That Can Fail Because of St. John’s Wort
Over 50 prescription drugs have documented, dangerous interactions with St. John’s Wort. Here are the ones you absolutely cannot mix:
- Immunosuppressants like cyclosporine, tacrolimus, and sirolimus. These are critical for transplant patients. St. John’s Wort can cause organ rejection.
- HIV medications like protease inhibitors (ritonavir, indinavir) and non-nucleoside reverse transcriptase inhibitors. Reduced levels mean the virus can come back strong.
- Oral contraceptives. The FDA and European Medicines Agency both warn: St. John’s Wort can make birth control fail. There are real cases of unintended pregnancies linked to this combo.
- Anticoagulants like warfarin. One patient’s INR (a measure of blood clotting) dropped from 2.5 to 1.4 in 10 days after starting St. John’s Wort. That’s a 44% drop in blood thinning power.
- Antidepressants like SSRIs and SNRIs. Mixing them can cause serotonin syndrome-agitation, rapid heart rate, high fever, seizures. It’s rare, but it kills.
- Pain meds like oxycodone, methadone, and tramadol. St. John’s Wort can reduce their pain-relieving effects, leaving patients in unnecessary pain.
- Statins like simvastatin and atorvastatin. Lower levels mean higher cholesterol, higher heart attack risk.
- Chemotherapy drugs like irinotecan and etoposide. Reduced effectiveness could mean cancer progression.
The European Medicines Agency says St. John’s Wort should never be used with any drug that has a narrow therapeutic index-meaning the difference between a safe dose and a toxic one is tiny. That’s exactly what these drugs are.
Why You Might Not Realize It’s Happening
Most people don’t connect the dots. You start taking St. John’s Wort for anxiety. A week later, your migraine meds stop working. You think you need a higher dose. You double it. Then your blood pressure drops too low. You go to the doctor. They check your meds. Nothing’s wrong. You’re taking everything as prescribed.
But here’s the hidden delay: It takes about 10 days for St. John’s Wort to fully induce those liver enzymes. And the effect doesn’t stop when you quit. It lingers for up to two weeks. So if you stop taking it before surgery or switch to a new drug, your body is still clearing meds faster than normal.
A 2017 study found that the average patient took 3 to 6 weeks to realize their medication wasn’t working because of St. John’s Wort. By then, damage could already be done.
What the Labels Don’t Tell You
In Europe, St. John’s Wort products must carry bold warnings about interactions with birth control, immunosuppressants, and blood thinners. In the U.S.? Not so much. The FDA doesn’t require pre-market approval for supplements. So you’ll find bottles with tiny print like “may interact with medications,” but no list. No specifics. No urgency.
Meanwhile, the European Medicines Agency has been clear since 2004: if you’re on anything with a narrow therapeutic window, don’t touch it. The U.S. Public Health Advisory from 2000 warned about interactions, but it didn’t change the market. St. John’s Wort is still sold everywhere-from grocery stores to Amazon.
And here’s the kicker: The supplement industry isn’t required to test for interactions. One study found that 60% of St. John’s Wort products on the market had hyperforin levels that varied by over 50% from what was listed on the label. So even if you think you’re taking a “safe” dose, you might be getting twice the interaction risk.
Who’s Most at Risk?
You might think, “I’m healthy. I don’t take anything serious.” But here’s the reality:
- Women aged 35 to 54 are the biggest users-exactly the group most likely to be on birth control, antidepressants, or thyroid meds.
- People with chronic conditions-diabetes, heart disease, HIV-are often on multiple meds. One extra herb can tip the balance.
- Older adults (65+) use it less, but that’s not because they’re safer. It’s because they’re on so many drugs, their doctors usually catch it.
And don’t assume your pharmacist knows. A 2021 survey found that nearly 40% of pharmacists didn’t routinely ask patients about herbal supplement use during medication reviews. They’re focused on prescriptions. Supplements? They’re an afterthought.

What Should You Do Instead?
If you’re considering St. John’s Wort for depression or anxiety, here’s what to do:
- Make a full list of every medication and supplement you take-prescription, over-the-counter, vitamins, herbs.
- Bring it to your doctor or pharmacist. Don’t just say, “I’m thinking of trying this herb.” Say, “I’m considering St. John’s Wort. What could it interfere with?”
- If you’re on any of the high-risk drugs listed above, skip it. Period.
- If you’re not on anything risky and your doctor approves it, start low (300 mg daily) and monitor for changes in how your other meds work.
- Consider alternatives. SAM-e and 5-HTP have far fewer interactions. Studies show they’re less effective for depression than St. John’s Wort, but they’re safer.
There’s also new research on low-hyperforin St. John’s Wort extracts. A 2022 study showed they reduce enzyme induction by 90%. But they’re not widely available yet. And they’re not labeled as “safe.” So don’t assume.
The Bottom Line
St. John’s Wort isn’t harmless. It’s not a gentle herb. It’s a drug-level modulator of your body’s detox system. And when you mix it with prescription meds, you’re playing Russian roulette with your health.
It’s not about being scared of natural remedies. It’s about being smart. Just because something is sold as a supplement doesn’t mean it’s safe. And just because it’s labeled “natural” doesn’t mean it doesn’t have powerful, dangerous effects.
If you’re thinking of using it, talk to someone who knows your full medical history. Don’t rely on a label. Don’t trust a Reddit post. And don’t assume your doctor knows you’re taking it-most don’t ask.
There’s a reason the American Society of Health-System Pharmacists predicts St. John’s Wort use will drop to under 2% of U.S. adults by 2030. It’s not because it doesn’t work. It’s because too many people got hurt using it without knowing the risks.
Your mood matters. But your life matters more.
Can St. John’s Wort make birth control fail?
Yes. Multiple case reports and studies confirm that St. John’s Wort reduces the effectiveness of oral contraceptives by increasing the metabolism of estrogen and progestin. Women have reported unexpected pregnancies after starting St. John’s Wort-even when taking birth control perfectly. The European Medicines Agency and FDA both warn about this interaction. If you’re using hormonal birth control, avoid St. John’s Wort entirely.
How long does it take for St. John’s Wort to affect other medications?
It takes about 10 days for St. John’s Wort to fully induce liver enzymes that break down other drugs. But the effect doesn’t stop when you quit. The enzyme levels stay elevated for up to two weeks after stopping St. John’s Wort. That means even if you stop taking it before surgery or switching meds, you’re still at risk during that two-week window.
Is St. John’s Wort safer than prescription antidepressants?
For mild to moderate depression, studies show St. John’s Wort can be as effective as some SSRIs, with fewer side effects like weight gain or sexual dysfunction. But it’s not safer overall. Its interaction profile is far more dangerous. While SSRIs have side effects, they don’t routinely cause organ rejection, birth control failure, or life-threatening drops in drug levels. The risk-benefit balance only favors St. John’s Wort if you’re not taking any other medications.
Can I take St. John’s Wort with vitamins or other supplements?
Some supplements are safe, but others aren’t. St. John’s Wort can interact with 5-HTP and L-tryptophan, increasing the risk of serotonin syndrome. It may also reduce the effectiveness of melatonin and certain B vitamins. Even “harmless” supplements like ginkgo biloba or garlic can increase bleeding risk when combined with St. John’s Wort. Always check with a pharmacist before mixing any supplement with St. John’s Wort.
What should I do if I’ve already taken St. John’s Wort with my prescription meds?
Stop taking St. John’s Wort immediately. Contact your doctor or pharmacist and tell them exactly what you’ve been taking and for how long. If you’re on a critical medication like an immunosuppressant, anticoagulant, or HIV drug, you may need blood tests to check drug levels. Don’t wait for symptoms. Even if you feel fine, the drug levels could already be dangerously low.
Are there any St. John’s Wort products that are safe to use with medications?
There are experimental low-hyperforin extracts that reduce enzyme induction by up to 90%, but they’re not widely available in the U.S. or Europe. No product on the market today is labeled as “safe for use with prescription drugs.” Even if a label claims “standardized extract,” it doesn’t mean it’s low-risk. Hyperforin levels vary wildly between brands. Until a regulated, tested, and clearly labeled low-interaction version becomes mainstream, assume all St. John’s Wort products carry risk.
Gran Badshah
December 30, 2025 AT 00:21Bro I took this stuff for 3 months last year while on my anxiety med. Thought it was chill. Then my heart started skipping like a broken record. ER visit later - my drug levels were in the toilet. Never again. Labels lie.
Ellen-Cathryn Nash
December 31, 2025 AT 16:17People still take this like it’s herbal tea? 😭 I swear, the moment someone says 'natural' and 'safe' in the same sentence, my BS detector goes full nuclear. This isn't wellness - it's medical roulette with a side of ignorance. If you're on anything important, don't be a lab rat for Big Supplement.
Samantha Hobbs
January 1, 2026 AT 13:39OMG I just found out my mom’s been taking this with her blood thinner. I freaked out and made her stop. She said it 'helped her mood' but now she’s scared to even say it out loud. Like... why isn’t this on the bottle? Like, BIG BOLD LETTERS??
Nicole Beasley
January 2, 2026 AT 10:27So if I took this with my birth control and got pregnant... is it my fault? 😅 I mean, I didn’t read the fine print. But also... why does the FDA let this even exist?? 🤦♀️
sonam gupta
January 3, 2026 AT 15:45Julius Hader
January 3, 2026 AT 20:01I used to be a big fan of St. John’s Wort - thought it was the answer to my low mood. Then I realized I was just replacing one problem with a dozen hidden ones. My doctor laughed when I told him I thought it was 'gentler.' He said, 'Son, it’s not gentle. It’s a saboteur.' And he was right.
Vu L
January 4, 2026 AT 18:01Yeah but what if you’re not on any meds? Then it’s just a fancy placebo with a side of liver stress. I’ve seen people take this for years and swear by it. Maybe the real problem isn’t the herb - it’s that we’ve turned every mood swing into a medical crisis.
Mimi Bos
January 5, 2026 AT 00:05so i took this for like 2 weeks last winter and my anxiety got better but then my antidepressant stopped working?? i thought i was just getting worse lol. i had no idea it was the herb. my pharmacist didn’t even ask about supplements. kinda scary how easy it is to mess up your whole system without meaning to 🥲
Payton Daily
January 6, 2026 AT 12:55Look. This isn’t about St. John’s Wort. It’s about the illusion of control. We want to fix our pain without doctors, without pills, without accountability. We want to be the hero of our own healing story. But biology doesn’t care about your intentions. It doesn’t care if you called it 'natural.' Your liver doesn’t have a soul. It doesn’t know you meant well. It just metabolizes. And when it does - you don’t get a second chance. This isn’t a warning. It’s a funeral notice for people who think they’re smarter than biochemistry.