Breast Cancer: Signs, Screening & Practical Help
Worried about breast cancer or helping someone who is? Early detection makes a big difference. About 1 in 8 women in the U.S. will develop invasive breast cancer in their lifetime, so knowing the basics helps you act fast and get the right care.
What should you watch for? The most common sign is a new lump or thickening in the breast or underarm. Also notice any nipple changes (inversion, discharge), persistent pain in one spot, or skin changes like dimpling or redness. A lump isn’t an automatic cancer diagnosis — many lumps are benign — but check it with a doctor if it’s new or different.
When to get screened
Screening shows problems before symptoms appear. Recommendations vary, but many doctors suggest starting regular mammograms around age 40. For most people, a mammogram every 1–2 years is common. If you have a strong family history or known gene changes (like BRCA), screening often starts earlier and may include MRI in addition to mammograms. Ask your provider what schedule fits your personal risk.
Self-checks can help you spot changes between screenings, but they don’t replace mammograms. If you feel something odd, call your clinic — faster evaluation means faster answers and treatment if needed.
What tests and treatments look like
If screening finds something, your doctor may order diagnostic images (targeted mammogram or ultrasound) and often a biopsy. A biopsy is the only way to confirm cancer and to learn the tumor’s type and grade — information that guides treatment.
Treatment depends on stage and tumor type. Common options include surgery (lumpectomy or mastectomy), radiation, chemotherapy, hormone therapy, and targeted drugs. Some people get a combination. Side effects vary by treatment, so ask your team about ways to manage nausea, fatigue, hair loss, and mood changes. Many centers offer nurse navigators, social workers, and rehab services to make care easier.
What should you ask your doctor? Key questions include: What stage and type is this? What are my treatment choices and goals? What side effects should I expect and how will they be managed? Should I see a genetic counselor? When can I get a second opinion? Keep a written list of questions and bring a friend or family member to appointments.
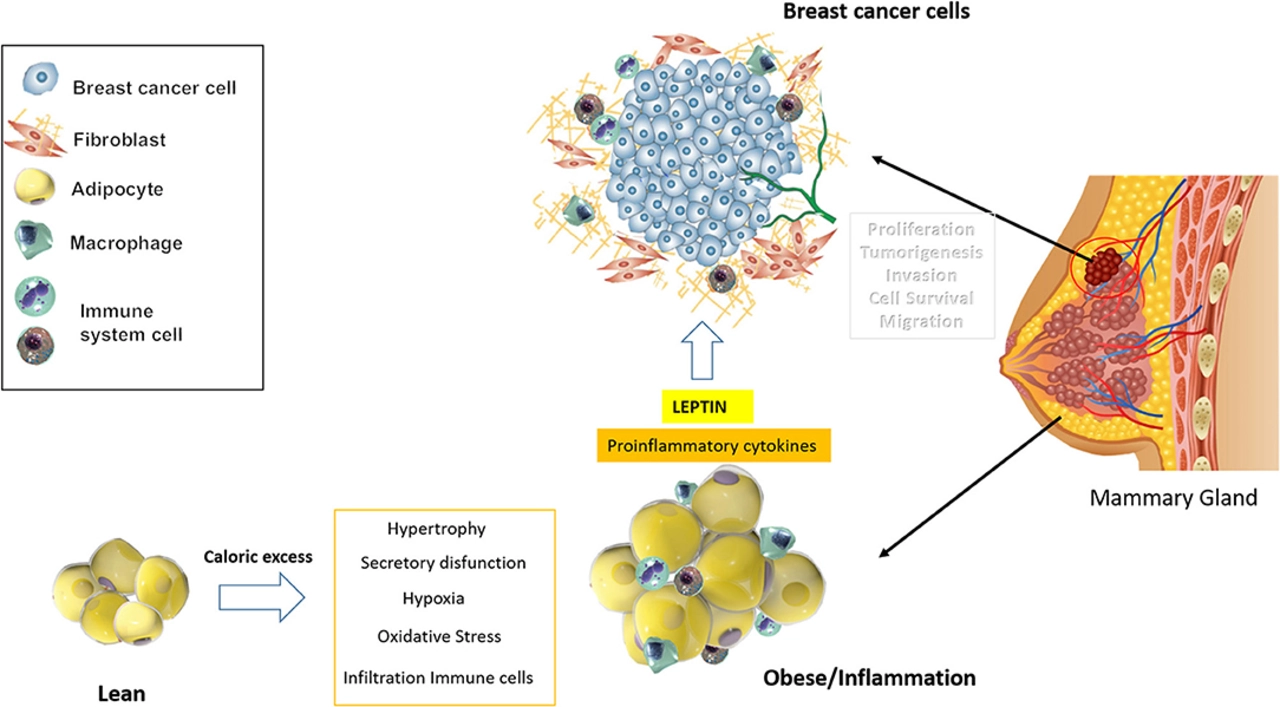
Looking after yourself matters. Aim for regular activity, maintain a healthy weight, limit alcohol, and get enough sleep. If you have a strong family history, get genetic testing and specialized screening. Emotional support is crucial — join a support group, talk with a counselor, or connect with peers online.
Need reliable resources? Start with your doctor and trusted cancer centers. For more practical health and medication guides, visit RX2Go.com. If something feels off, don’t wait — early checks save lives and make treatment simpler.