Hormone receptor-positive: what you need to know
Hormone receptor-positive sounds technical — what does it mean for you? In simple terms, it means cancer cells have proteins that latch onto hormones like estrogen or progesterone and use them to grow. That detail changes how doctors test, treat, and follow the disease.
A hormone receptor test comes from a biopsy. Pathologists stain tumor tissue to see if estrogen receptors (ER) or progesterone receptors (PR) are present. Positive results are reported as percentages or scores. A high percentage usually means the tumor is more likely to respond to hormone-blocking treatments. If your report says ER-positive, PR-positive, or hormone receptor-positive, that’s a clue your care team will use to plan therapy.
Hormone-blocking treatments are the main plan for hormone receptor-positive disease. For premenopausal people, tamoxifen is a common option. It blocks estrogen in breast tissue. For postmenopausal people, aromatase inhibitors such as anastrozole, letrozole, or exemestane lower estrogen levels and often work better. Doctors sometimes combine endocrine therapy with targeted drugs like CDK4/6 inhibitors (palbociclib, ribociclib, abemaciclib) or mTOR inhibitors to improve results, especially in advanced cases.
Surgery and radiation still matter. If the tumor is operable, surgery removes the bulk of disease and gives more tissue for testing. Radiation lowers the chance of local return. Hormone therapy usually follows to reduce distant recurrence risk. In some cases, hormone therapy is given before surgery to shrink the tumor so breast-conserving surgery becomes possible.
Side effects and daily life should be front and center in planning. Tamoxifen can cause hot flashes and raise blood clot risk. Aromatase inhibitors often bring joint pain and bone thinning, so doctors check bone density and may add calcium, vitamin D, or bone-targeted drugs. CDK4/6 inhibitors can cause low blood counts or diarrhea; labs are monitored regularly. Talk openly with your team about symptoms — small changes matter and often have easy fixes.
How long will treatment last? For early-stage hormone receptor-positive disease, endocrine therapy commonly runs five to ten years. That long-term plan cuts the risk of late recurrence. For advanced disease, endocrine therapy aims to control growth and preserve quality of life; plans are more flexible and adjusted over time.
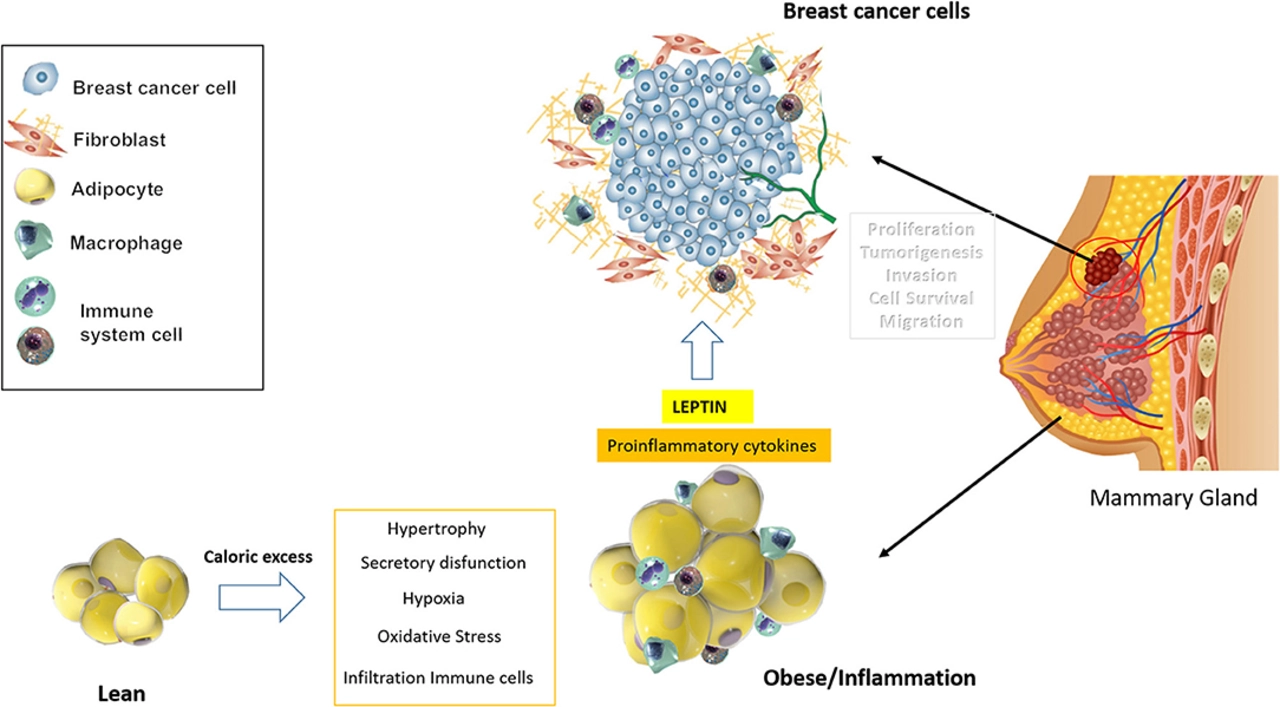
Follow-up is ongoing. Expect regular visits, bloodwork, and imaging as needed. Lifestyle steps also help: staying active, keeping a healthy weight, limiting alcohol, and eating a balanced diet can lower recurrence risk. Mental health matters too — support groups, counseling, or patient networks help when treatment feels heavy.
Ask the right questions at your appointments: Which receptors are positive and by what score? What are my endocrine therapy options? Will I need targeted drugs or chemo? What side effects should I expect and how do we manage them? Who monitors my bone health and blood counts?
If you want deeper reading, check our guides on specific drugs, side effects, or how to get medicines safely online. Knowing the hormone receptor status gives real choices — and a clear path to personalized care. If unsure, bring your pathology report and ask for a copy to review with your doctor.