Medication Errors: What They Are, How They Happen, and How to Stop Them
When you take a pill, you expect it to help—not hurt. But medication errors, mistakes in prescribing, dispensing, or taking drugs that lead to harm. Also known as drug safety incidents, they’re one of the most common causes of preventable hospital visits in the U.S. These aren’t just rare accidents. They happen every day: a nurse grabs the wrong bottle, a pharmacist misreads a script, a patient mixes pills without knowing the risks, or a doctor prescribes a drug that clashes with another. And it’s not just about dosage. It’s about timing, timing, and knowing what’s in the bottle.
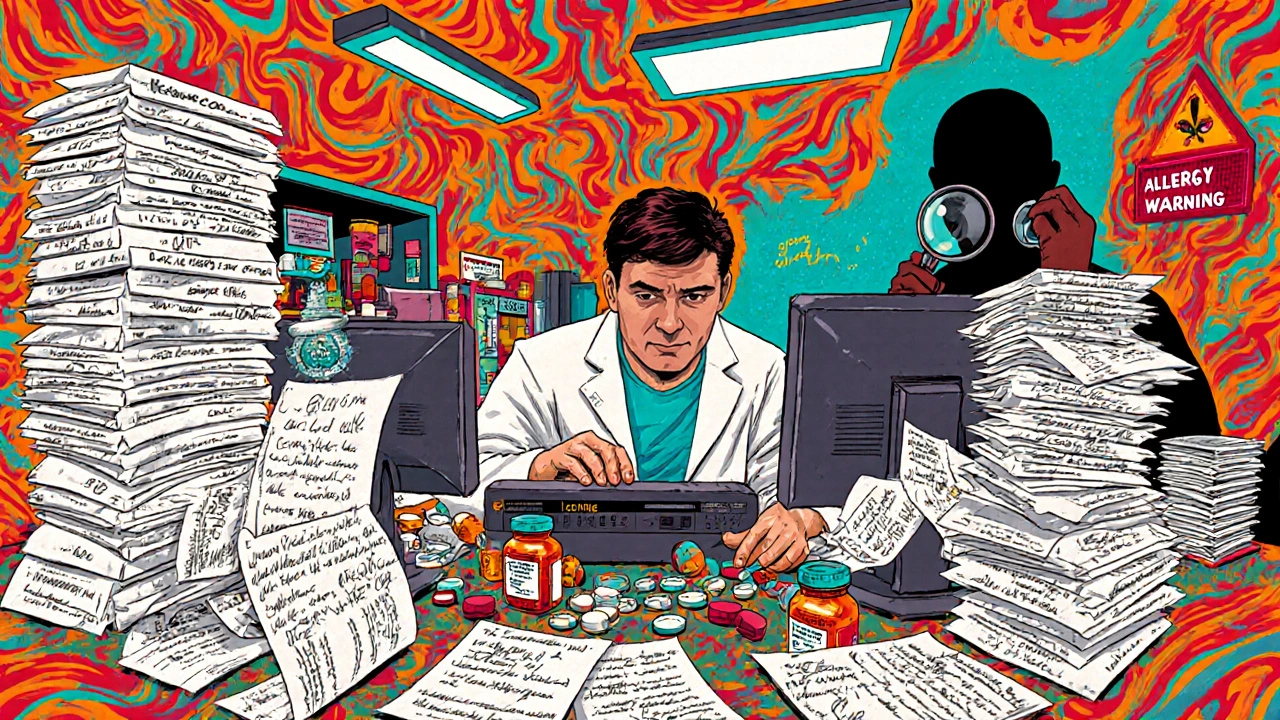
Prescription mistakes, errors that start when a doctor writes or enters a drug order incorrectly are often the first step. Maybe the handwriting was unclear. Maybe the system auto-filled the wrong dose. Maybe the patient has kidney problems, and the doctor didn’t check. Then comes pharmacy errors, when the pharmacy gives you the wrong drug, wrong strength, or wrong instructions. A 2023 study found that nearly 1 in 20 prescriptions filled at community pharmacies had some kind of error—most of them caught before the patient left, but not all. And then there’s the patient side: taking meds with grapefruit juice, skipping doses because they’re expensive, or doubling up because you forgot if you already took it. These aren’t just "human errors." They’re system failures.
Some drugs are especially dangerous if messed with. Medication safety becomes critical with things like warfarin, lithium, or insulin—tiny changes in dose can mean hospitalization or death. That’s why expiration dates matter for NTI drugs. That’s why you need to talk to your pharmacist about supplements. That’s why flying with insulin or CBD requires knowing TSA rules. And that’s why switching from brand to generic isn’t always as simple as saving money—it’s about making sure your body reacts the same way. These aren’t abstract risks. They show up in real stories: an elderly person confused from low sodium because of an SSRI, a diabetic with swelling because diuretics weren’t adjusted for kidney disease, or someone with vitiligo using a skin cream they weren’t told could interact with other meds.
You don’t need to be a medical expert to protect yourself. But you do need to ask questions. Know your meds. Check the label. Keep a list. Bring it to every appointment. Talk to your pharmacist—not just when you pick up a script, but when you have a question. These aren’t just tips. They’re survival tools in a system that’s still full of holes. Below, you’ll find real, practical guides on exactly how these mistakes happen, how to catch them, and how to make sure you or someone you care about doesn’t become a statistic.