The Intricate Balance: Diabetes and Your Urinary Health
Let's delve into some serious stuff here. As a male blogger bearing the charming name Dorian, I may not immediately strike you as an authority on matters of the bladder and urinary tract. But as my son Emmett always tells his friends when they tease him about his "cool blogger dad" (yes, that's me!), I am full of surprising knowledge. So stick around, we're about to explore the intersection between diabetes and muscle spasms in the bladder and urinary tract.
The Sneaky Sides of Diabetes
As we venture through this discussion, remember it's not just about sugars and diet, but it surely starts there. Diabetes is that sneaky little devil that loves to highjack our bodies when we're not paying attention to our blood sugar levels. In type 2 diabetes, for instance, the body resists insulin or doesn't produce enough. This leads to elevated blood glucose levels. That glucose needs to go somewhere, and where does it eventually sit? Well, it parks itself in various organs and tissues, causing a disruption in their functionality. Directing my gaze towards the bladder and urinary tract, these are prime targets in the crosshairs of diabetes.
A Stumble in the Dance Club: Muscle Spasms
Let's bring some rhythm into the discussion. Think of your bladder as a classic, cool dance club. The muscular walls of the bladder are in a constant rhythm, expanding and contracting to store and pass urine. Now imagine your bladder's sweet dance moves getting interrupted. That's what muscle spasms are like. But how does diabetes come into play here? Well, sit tight because I'm about to shed some light on this complex disco.
Party Pooper: Diabetes Interrupts the Bladder Boogie
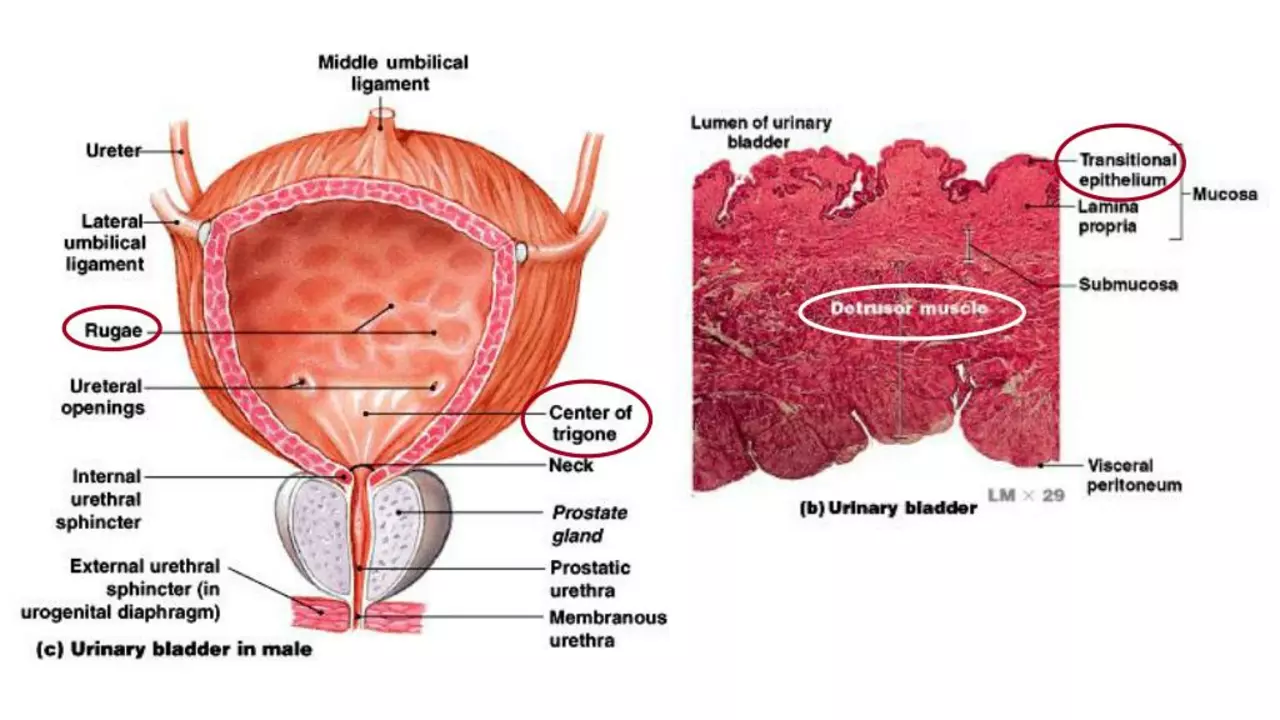
High glucose levels in your body, caused by diabetes, can be a real party pooper. They cause nerve damage in many parts of your body, including the bladder, leading to a variety of urinary problems. Frequent urination, an intense urge to pee, and trouble emptying your bladder - all these can result from this nerve damage, known as diabetic neuropathy. Now, not to scare you, but this can lead to bladder damage, meaning your bladder's smooth dance routine is disrupted. Yes, this is when muscle spasms come in, causing involuntary movements that can lead to symptomatic issues like urinary incontinence. Can you see the intricate link here? Diabetes, nerve damage, muscle spasms, and bladder issues, all interconnected in an unfortunate chain of events.
Deciphering the Signs: Symptoms of Bladder Spasms
So, how do you know if your bladder is having an involuntary jive, twisted by diabetes? Symptoms to watch out for include sudden, strong urges to urinate, even if your bladder isn't full. You may experience urinary leakage or discomfort in your lower abdomen. Pain below your belly button, a burning sensation during urination, and waking up multiple times at night to pee - these could all be signs that your bladder muscles are indeed throwing off their rhythm. Pretty pesky, isn't it?
Keeping the Rhythm Going: Management and Prevention
Alright, enough about the problems! Let's turn the table and discuss solutions - keeping that bladder boogie smoothly going! Managing your diabetes effectively is the best approach. This involves maintaining a healthy diet, regular exercise, and monitoring your blood glucose levels. And don't forget to shake it up with medication if prescribed by your beloved healthcare provider. Regular check-ups are key too, making sure your disco isn't interrupted by pesky bladder spasms.
A Little Extra Move: Lifestyle Adaptations
To prevent innocent trips to the toilet from turning into unwelcome adventures, a few lifestyle adaptations can be helpful. These might include adjusting your fluid intake and diligently scheduling toilet trips. A high-fiber diet is also beneficial, since constipation can pressure your bladder and enhance spasm activity. And if you're up for it, don't shy away from pelvic floor exercises. They can be fantastic to support your bladder muscles and keep them in rhythm.
Curveballs and Silver Linings
Life's full of curveballs, and sometimes, diabetes might be one for you. But hey, every cloud has a silver lining! Understanding the relationship between diabetes and muscle spasms in the bladder and urinary tract is one step closer to managing effectively and keeping the rhythm of life going. Sure, diabetes might make your bladder do the funky chicken, but with the right knowledge and strategies, you can take back control and keep the dance lively and under your lead.
king singh
July 31, 2023 AT 18:26Managing blood sugar is the foundation; stable glucose reduces the risk of neuropathy that can trigger bladder spasms.
Adding regular pelvic floor exercises can strengthen the muscle tone and help regulate involuntary contractions.
Staying hydrated but not overloading the bladder at once also gives the organ a chance to recover.
Overall, a balanced lifestyle works as both prevention and treatment.
Adam Martin
August 5, 2023 AT 15:00Oh, so you’ve discovered that diabetes can mess with your bladder – groundbreaking, right? The poor little organ suddenly decides it’s a fire‑drill drill sergeant, shouting “urinate now!” at the most inconvenient moments. That’s because hyperglycemia loves to sabotage the autonomic nerves that keep the detrusor muscle on a sensible schedule. When those nerves are fried, the bladder’s rhythmic dance turns into a chaotic rave. Imagine trying to concentrate at work while your pelvis is hosting an unexpected rave party. The result? You’re sprinting to the restroom like it’s a 100‑meter dash, and sometimes you don’t even make it in time. Meanwhile, the body’s attempt to flush excess glucose through urine only adds fuel to the fire, irritating the bladder lining further. The combination of nerve damage, altered bladder compliance, and increased urinary frequency is a perfect storm for involuntary spasms. It gets even more fun when you factor in that the same diabetic neuropathy can affect the sphincter, turning smooth coordination into a clumsy stumble. Physicians often prescribe anticholinergics, but those come with their own baggage of dry mouth and constipation, which can be just as annoying. Lifestyle adjustments, like limiting caffeine and alcohol, can tip the scales slightly back toward normalcy. Staying on top of HbA1c levels isn’t just about preventing foot ulcers; it’s also about giving your bladder a fighting chance. Pelvic floor physical therapy can re‑educate the muscles, teaching them not to overreact. In short, think of diabetes as the uninvited DJ who keeps changing the beat, and you as the dancer who just wants a steady groove. So, keep that glucose in check, follow up with your urologist, and maybe your bladder will finally learn some better moves.
Ryan Torres
August 10, 2023 AT 11:35🛑 Wake up and realize the pharma giants don’t want you to know how sugar spikes are secretly wired to your bladder’s nervous system! They hide the fact that every high‑glycemia episode plants a tiny spy in your detrusor muscle, ready to sabotage you at night. 👀 That’s why you keep getting up at 3 AM, because the system they designed forces you to thirst for control while they control the rest. Stop trusting mainstream “medical advice” and start looking at the data they hide in the fine print. 💥
shashi Shekhar
August 15, 2023 AT 08:09Yeah, because nothing says “healthy lifestyle” like a bladder that does the cha‑cha whenever you forget your insulin.
Marcia Bailey
August 20, 2023 AT 04:43Great points on staying hydrated; just remember to drink a glass of water 30 minutes before bedtime to reduce nighttime trips 😊. Incorporating moderate aerobic exercise can improve insulin sensitivity, which in turn eases the pressure on bladder nerves. Don’t forget to schedule regular check‑ups with your urologist to catch any early signs of neuropathy.
Hannah Tran
August 25, 2023 AT 01:17From a urodynamic perspective, diabetic autonomic neuropathy leads to detrusor overactivity, which manifests as urgency‑frequency syndrome. Implementing antimuscarinic agents can mitigate involuntary detrusor contractions, though clinicians must monitor for anticholinergic burden. Concurrently, optimizing glycemic control reduces polyuria, thereby decreasing bladder wall stretch and subsequent spasm frequency. It’s essential to conduct a comprehensive cystometric evaluation to tailor therapy appropriately. By integrating pelvic floor biofeedback with pharmacotherapy, patients often achieve symptom remission.
Dhananjay Sampath
August 29, 2023 AT 21:52First, maintain strict glycemic control, because, as we all know, high glucose levels directly impair autonomic nerves, leading to detrusor instability; second, schedule regular voiding intervals, which can condition the bladder muscle, preventing over‑reactivity; third, engage in pelvic floor strengthening exercises, such as Kegels, to support urethral closure, and finally, consult a urologist for personalized treatment plans, including possible pharmacologic options.
kunal ember
September 3, 2023 AT 18:26It is academically accurate to state that the pathophysiological cascade originating from chronic hyperglycemia induces a decrement in the myelination of peripheral autonomic fibers, which, in turn, compromises the coordinated contraction‑relaxation cycle of the detrusor muscle, thereby precipitating involuntary spasms; consequently, patients often present with a symptom complex characterized by nocturia, urgency, and occasional stress incontinence, all of which merit a thorough urological assessment. Moreover, integrating lifestyle modifications-such as a low‑glycemic-index diet, consistent aerobic activity, and mindful fluid timing-serves to ameliorate the underlying metabolic derangements, which are the primary drivers of neurogenic bladder dysfunction. In clinical practice, the utilization of urodynamic studies provides quantifiable metrics for detrusor pressure and compliance, guiding the selection of therapeutic agents ranging from anticholinergics to beta‑3 agonists, each with its own pharmacodynamic profile. Therefore, a multidisciplinary approach that bridges endocrinology and urology is indispensable for optimizing patient outcomes.
Kelly Aparecida Bhering da Silva
September 8, 2023 AT 15:00Don’t be fooled by the “global health” agenda that downplays the link between sugar addiction and bladder control-our leaders know that keeping the populace dependent on cheap carbs guarantees a compliant workforce. The real battle is taking back our health, starting with cutting out the processed sweeteners that sabotage our nerves and leave us at the mercy of a broken system.
Michelle Dela Merced
September 13, 2023 AT 11:35OMG, my bladder turned into a drama queen after a single high‑sugar binge! 😱 It was like an unexpected fireworks show at 2 AM, and I couldn’t even get any sleep.
Mark Conner
September 18, 2023 AT 08:09Enough with the excuses-control your sugar or your bladder will betray you.
Charu Gupta
September 23, 2023 AT 04:43It is imperative, therefore, to underscore the significance of stringent glycemic regulation in the prophylaxis of neurogenic bladder spasms. Such diligence not only mitigates autonomic neuropathy but also preserves the integrity of detrusor compliance. 📚
Abraham Gayah
September 28, 2023 AT 01:17Well, I suppose the bloke’s “expertise” on bladder beats is as deep as a puddle after a rainstorm-quite the splash, really.
rajendra kanoujiya
October 2, 2023 AT 21:52While many claim diabetes is the main culprit for bladder spasms, I argue that overhydration and excessive caffeine intake are equally, if not more, responsible for provoking involuntary detrusor activity.
Caley Ross
October 7, 2023 AT 18:26Just a heads‑up: keeping a bladder diary can reveal patterns you might otherwise miss, making it easier to discuss specific triggers with your doctor.