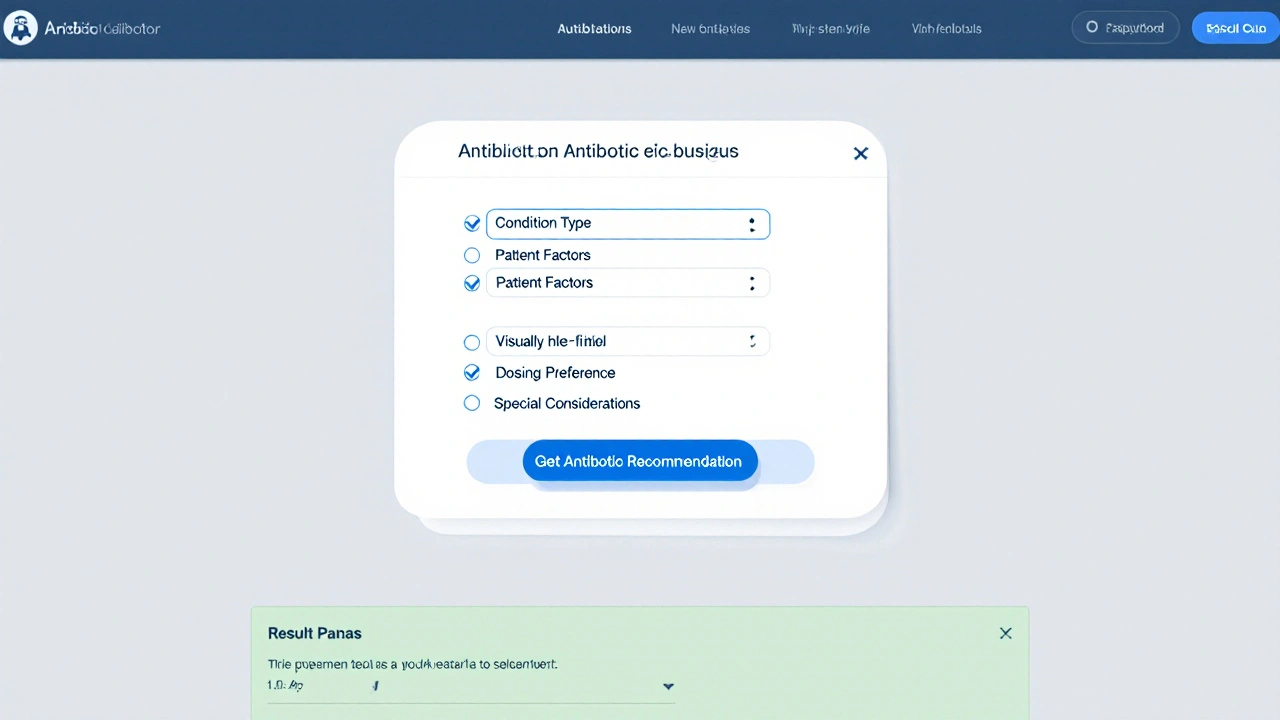
Antibiotic Selector Tool
Select your condition and preferences to get a recommended antibiotic:
Condition Type
Patient Factors
Dosing Preference
Special Considerations
Recommended Antibiotic:
Why This Choice:
Quick Take
- Zithromax (azithromycin) is a once‑daily macrolide with a short course but can cause GI upset and interacts with certain meds.
- Amoxicillin offers a narrower spectrum, cheap price, and is safe in pregnancy.
- Doxycycline works well for atypical bugs, but photosensitivity is a common drawback.
- Clarithromycin is a close macrolide cousin; it shares many side effects but has a higher pill burden.
- Levofloxacin provides broad coverage but carries serious tendon and QT‑interval risks.
When doctors prescribe a broad‑spectrum antibiotic, Zithromax is the brand name for azithromycin, a macrolide antibiotic that blocks bacterial protein synthesis. It’s taken once daily, usually for 3‑5days, and is used for respiratory, skin and certain sexually transmitted infections.
How Zithromax Works and When It’s Used
Azithromycin binds to the 50S ribosomal subunit, halting the growth of susceptible bacteria. Because it accumulates inside cells, a short regimen can sustain therapeutic levels after dosing stops. Common indications include community‑acquired pneumonia, strep throat, chlamydia, and sinus infections.
Typical adult dosing is 500mg on day1 followed by 250mg daily for four more days, although a single 1g dose is sometimes used for sexually transmitted infections. The convenience of once‑daily dosing makes it popular, especially for patients who dislike multiple pills.
Key Criteria for Choosing an Antibiotic
Before swapping drugs, weigh these factors:
- Spectrum of activity - does the drug cover the suspected bug?
- Dosing convenience - once daily vs. multiple times daily.
- Side‑effect profile - GI upset, photosensitivity, tendon risk, etc.
- Resistance patterns - local antibiograms can tip the scales.
- Cost and insurance coverage - generic options are often cheaper.
- Special populations - pregnancy, children, liver disease.
Top Alternatives to Zithromax
Each alternative below is introduced with a brief definition that includes its drug class, typical uses, and a key attribute.
Amoxicillin is a penicillin‑type beta‑lactam antibiotic that interferes with bacterial cell‑wall synthesis. It’s first‑line for otitis media, uncomplicated urinary tract infections, and many streptococcal infections.
Doxycycline is a tetracycline derivative that inhibits protein synthesis by binding the 30S ribosomal subunit. It shines against atypical pneumonia, Lyme disease, and acne.
Clarithromycin is another macrolide that, like azithromycin, blocks the 50S ribosomal subunit. It’s often chosen for Helicobacter pylori eradication and some respiratory infections.
Levofloxacin is a fluoroquinolone that hampers DNA gyrase and topoisomerase IV, preventing bacterial DNA replication. It covers a very broad range, from complicated UTIs to severe community‑acquired pneumonia.
Cefdinir is a third‑generation cephalosporin that disrupts cell‑wall formation. It’s useful for sinusitis, bronchitis, and skin infections when penicillins can’t be used.
Clindamycin is a lincosamide antibiotic that also targets the 50S ribosomal subunit, especially against anaerobes. It’s often a fallback for cellulitis or bone infections in penicillin‑allergic patients.

Side‑by‑Side Comparison
| Drug | Class | Typical Uses | Dosing Frequency | Common Side Effects | Resistance Concerns | Average Monthly Cost (US) |
|---|---|---|---|---|---|---|
| Zithromax (Azithromycin) | Macrolide | Respiratory infections, chlamydia, skin infections | Once daily (3‑5days) | Diarrhea, nausea, abdominal pain | Increasing macrolide resistance in Streptococcus pneumoniae | $20‑$30 (brand) / $8‑$12 (generic) |
| Amoxicillin | Penicillin (β‑lactam) | Otitis media, sinusitis, streptococcal pharyngitis | 2‑3 times daily | Rash, mild GI upset | β‑lactamase producing H. influenzae | $5‑$10 |
| Doxycycline | Tetracycline | Atypical pneumonia, Lyme disease, acne | Once or twice daily | Photosensitivity, esophageal irritation | Variable; often low for atypicals | $12‑$18 |
| Clarithromycin | Macrolide | H. pylori regimen, bronchitis | Twice daily | Taste disturbance, GI upset, drug interactions | Similar to azithromycin resistance patterns | $15‑$22 |
| Levofloxacin | Fluoroquinolone | Severe pneumonia, complicated UTIs | Once daily | Tendon rupture, QT prolongation, CNS effects | Rising resistance in E. coli, Pseudomonas | $25‑$35 |
| Cefdinir | Cephalosporin (3rd gen) | Sinusitis, bronchitis, skin infections | Once daily | Diarrhea, rash, possible C. difficile risk | Some ESBL‑producing organisms resistant | $18‑$25 |
| Clindamycin | Lincosamide | Anaerobic infections, bone/joint infections | 3‑4 times daily | High C. difficile colitis risk, metallic taste | Often effective against MRSA | $20‑$30 |
When Zithromax Is the Right Choice
- You need a short, once‑daily course (e.g., travel‑related diarrhea or chlamydia).
- The suspected pathogen is known to be susceptible to macrolides.
- The patient has a penicillin allergy but no macrolide cross‑reactivity.
- Adherence is a concern; fewer pills improve completion rates.
When an Alternative Is Preferable
Consider swapping if any of these apply:
- Documented macrolide resistance in your region’s antibiogram.
- Severe gastrointestinal intolerance to azithromycin.
- Pregnancy: amoxicillin or cefdinir are safer choices.
- Patient is on a medication that strongly interacts with macrolides (e.g., certain statins, ergotamines).
- Infection type falls outside azithromycin’s spectrum, such as Pseudomonas or MRSA, where levofloxacin or clindamycin may be needed.
Practical Tips for Using Any Antibiotic
- Finish the full prescribed course, even if symptoms improve.
- Take the dose with a full glass of water; avoid lying down for 30minutes to reduce esophageal irritation.
- Watch for allergic reactions: hives, swelling, difficulty breathing.
- Check for drug‑drug interactions-especially with macrolides and fluoroquinolones.
- Store the medication at room temperature, away from moisture, unless refrigeration is specified.
Frequently Asked Questions
Can I take Zithromax if I’m allergic to penicillin?
Yes. Azithromycin belongs to the macrolide class, which is chemically distinct from penicillins. Most penicillin‑allergic patients tolerate it, but cross‑reactivity can occur in rare cases of multiple drug allergies.
Why does my doctor sometimes prescribe a single 1g dose of Zithromax?
A one‑time 1g dose delivers a high initial concentration that clears certain sexually transmitted infections quickly. It simplifies adherence for patients who might forget a multi‑day schedule.
Is doxycycline better for acne than azithromycin?
For inflammatory acne, doxycycline is generally preferred because it targets the bacteria associated with acne and has a well‑studied dosing regimen. Azithromycin can be used when doxycycline is contraindicated, but evidence of its effectiveness is weaker.
What should I watch for with levofloxacin?
Serious side effects include tendon rupture (especially in older adults or those on steroids), QT‑interval prolongation, and central‑nervous‑system disturbances like dizziness or seizures. Stop the drug and seek medical help if you notice sudden joint pain or heart palpitations.
How do I know if my infection is resistant to azithromycin?
If symptoms persist after completing the full course, or if you develop a new fever, contact your provider. They may order a culture and sensitivity test to identify the exact bug and its antibiotic susceptibility.
Adam Shooter
September 30, 2025 AT 21:58From an evidence‑based perspective, the pharmacokinetic profile of azithromycin is dramatically overrated in popular discourse; its tissue accumulation is often mischaracterized as universally advantageous, overlooking the nuanced interplay with intracellular pathogens and host immune modulation. Moreover, the cost‑benefit calculus fails to account for the burgeoning macrolide resistance rates documented in multiple surveillance studies. The simplistic, once‑daily dosing convenience argument is, frankly, a reductive marketing ploy that sidesteps the essential principle of antimicrobial stewardship.
Shanmughasundhar Sengeni
October 6, 2025 AT 04:38The post's emphasis on convenience neglects the real-world implications of suboptimal dosing intervals, especially in regions where dosing adherence cannot be assumed. A physician's decision matrix must integrate local susceptibility patterns, not just the allure of a five‑day regimen.
ankush kumar
October 11, 2025 AT 11:18Let me break this down in a way that’s easy to follow. First, azithromycin’s long half‑life is a double‑edged sword: it allows for shorter courses, but it also means sub‑therapeutic levels linger, potentially fostering resistance.
Second, when you compare the spectrum, macrolides miss many gram‑negative organisms that a beta‑lactam would hit.
Third, side‑effects like GI upset are not trivial; they can lead patients to discontinue therapy prematurely.
Fourth, the drug–drug interaction profile of azithromycin is often underappreciated; it inhibits CYP3A4 and can elevate levels of statins, leading to myopathy.
Fifth, in pregnant patients, while azithromycin is relatively safe, amoxicillin remains the gold standard for many infections due to its extensive safety data.
Sixth, cost considerations matter: generics of amoxicillin are dramatically cheaper than brand‑name azithromycin, which can affect adherence in low‑income populations.
Seventh, resistance trends show an upward trajectory in Streptococcus pneumoniae, limiting azithromycin’s utility in community‑acquired pneumonia.
Eighth, clinicians should prioritize culture and sensitivity when possible, rather than defaulting to a broad‑spectrum agent.
Ninth, the notion that “once‑daily is always better” ignores patient-specific factors like renal or hepatic impairment that alter drug clearance.
Tenth, in the era of antimicrobial stewardship, preserving the efficacy of all antibiotic classes is paramount.
Eleventh, consider the ecological impact: widespread azithromycin use has been linked to shifts in gut microbiota composition.
Twelfth, for skin infections, especially those involving MRSA, clindamycin or doxycycline often provide better coverage.
Thirteenth, the convenience factor should never outweigh the principle of targeted therapy based on likely pathogens.
Fourteenth, the table in the article nicely summarizes the trade‑offs, but real‑world decision‑making requires more nuance.
Fifteenth, ultimately, the “best” antibiotic is the one that treats the infection effectively while minimizing collateral damage to the patient and the microbiome.
Cameron White
October 16, 2025 AT 17:58Azithromycin sounds cool but the government’s behind it.
Amélie Robillard
October 22, 2025 AT 00:38😂 Totally get the convenience vibe, but if you’ve got a pen‑allergy, the macrolide family can still give you a surprise rash. Always double‑check with your doc before you self‑medicate.
Fae Wings
October 27, 2025 AT 06:18Honestly, the biggest win here is the emphasis on finishing the full course. I’ve seen too many memes about “stop when you feel better” that end in relapse and tougher infections.
Anupama Pasricha
November 1, 2025 AT 12:58Just a heads‑up: if you’re dealing with acne, doxycycline still beats azithromycin in most guidelines, unless you’ve got a contraindication. Keep that in mind when you’re scrolling through the options.
April Yslava
November 6, 2025 AT 19:38Great info.
Daryl Foran
November 12, 2025 AT 02:18Look, if you’re reading this, you probably think you can outsmart your doctor. Trust me, the “once‑daily” hype is just a way to get you to buy brand‑name pills, not a medical necessity.
Dervla Rooney
November 17, 2025 AT 08:58I appreciate the thorough breakdown, but a few additional points deserve attention. First, while azithromycin’s tissue penetration is advantageous for intracellular pathogens, it also means prolonged exposure of commensal flora to sub‑inhibitory concentrations, which can select for resistant strains over time.
Second, the interaction with proton‑pump inhibitors can reduce absorption, diminishing its efficacy in certain patient populations.
Third, for patients on warfarin, azithromycin can amplify anticoagulant effects, necessitating closer INR monitoring.
Lastly, the table’s cost column doesn’t reflect insurance formularies, which heavily influence out‑of‑pocket expenses.
Johnny Ha
November 22, 2025 AT 15:38Yo, the article missed the fact that levofloxacin’s tendon risk is a myth spread by pharma. Real data shows it’s comparable to other antibiotics.
Mary Cautionary
November 27, 2025 AT 22:18While the comparative table is useful, it could benefit from a more nuanced discussion of pharmacodynamics, especially the post‑antibiotic effect observed with macrolides versus beta‑lactams.
Crystal Newgen
December 3, 2025 AT 04:58Good summary, but remember to always factor in patient adherence; a simpler regimen often trumps a theoretically superior drug.
Hannah Dawson
December 8, 2025 AT 11:38Is it just me, or does everyone forget to mention that azithromycin can cause QT prolongation when combined with other meds? That’s a serious safety gap.
Julie Gray
December 13, 2025 AT 18:18Given the current epidemiological data on macrolide resistance, clinicians should be circumspect about defaulting to azithromycin for community‑acquired pneumonia without confirmation of susceptibility.
Lisa Emilie Ness
December 19, 2025 AT 00:58Short and sweet: cost matters.
Emily Wagner
December 24, 2025 AT 07:38From a philosophical angle, antibiotics embody the tension between humanity’s desire for immediate resolution and the long‑term ecological consequences of microbial selection pressures.
Mark French
December 29, 2025 AT 14:18In my experience, patients value clear instructions over drug class minutiae; a well‑explained dosing schedule can improve outcomes more than any pharmacological nuance.
Daylon Knight
January 3, 2026 AT 20:58Wow, such a thorough guide! It's like the Swiss Army knife of antibiotic decisions-except it doesn't have the tiny scissors for cutting through insurance jargon.