Central Diabetes Insipidus – What It Is and How to Manage It
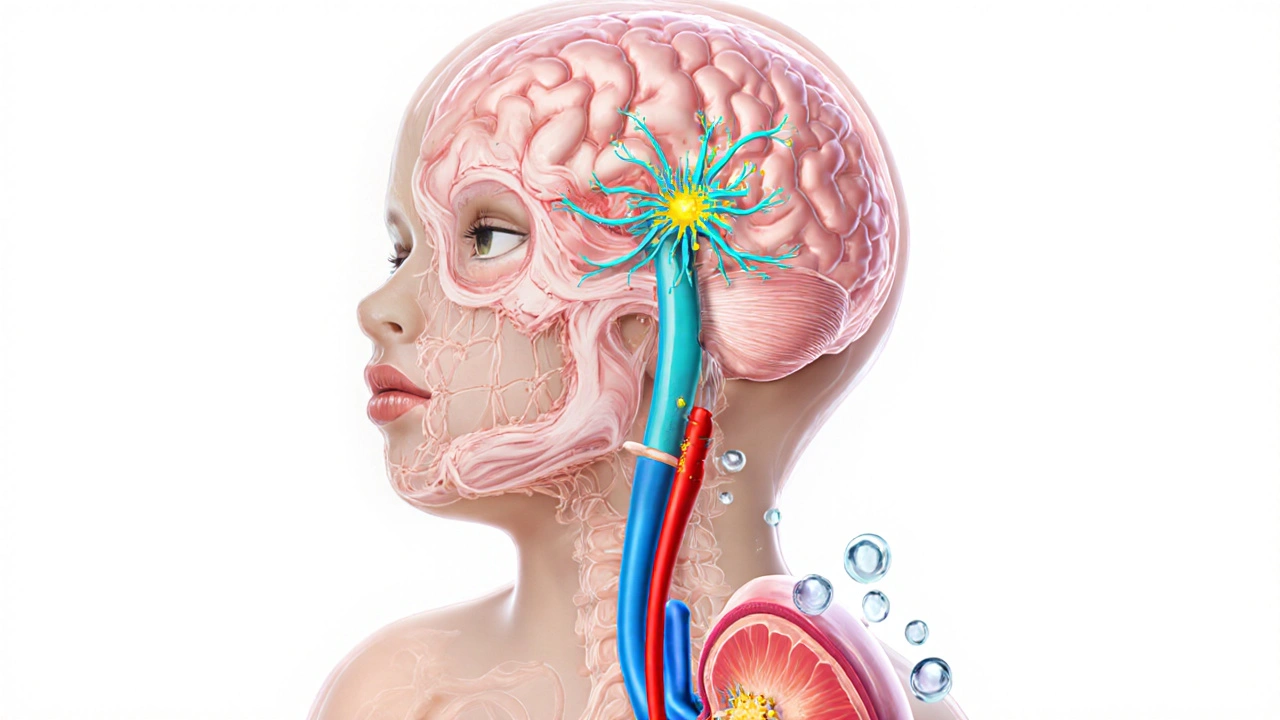
Imagine waking up and needing to run to the bathroom every hour – that’s what missing a single hormone can feel like. When working with Central Diabetes Insipidus, a rare condition where the brain fails to produce enough antidiuretic hormone (ADH). Also known as CDI, it stems from a problem in the hypothalamus, the brain region that makes ADH, or the pituitary gland that stores and releases it. Without adequate ADH, the kidneys can’t re‑absorb water, leading to massive urine output and unquenchable thirst.
Because the body can’t keep water, people with central diabetes insipidus often notice polyuria – drinking a lot and peeing hundreds of milliliters each hour. This creates a risk of high blood sodium (hypernatremia) if fluids aren’t replaced quickly. Doctors confirm the diagnosis with a water deprivation test, which measures how urine concentration changes when fluid intake is limited. If the kidneys still can’t concentrate urine, the next step is an ADH analog challenge: giving a dose of desmopressin, a synthetic vasopressin that mimics the missing hormone. A rapid drop in urine volume after desmopressin signals central, not nephrogenic, diabetes insipidus. The test not only tells you the type, it also helps tailor the right dose for long‑term management.
Treatment revolves around replacing the missing hormone and adjusting daily habits. Most patients stay on low‑dose desmopressin taken orally, nasally, or as a melt‑away tablet, which reduces urine output to near‑normal levels and quells thirst. Regular monitoring of blood sodium and weight ensures the dose isn’t too high, which could cause water retention. Lifestyle tweaks – drinking water before you feel thirsty, using a bathroom schedule, and checking urine color – complement medication. With proper care, central diabetes insipidus becomes a manageable condition rather than a daily crisis. Below you’ll find articles that dive deeper into causes, diagnostic tricks, medication choices, and real‑world tips for living with this hormone‑related disorder.