Chronic Kidney Disease Fluid Overload: Causes, Risks, and What You Can Do
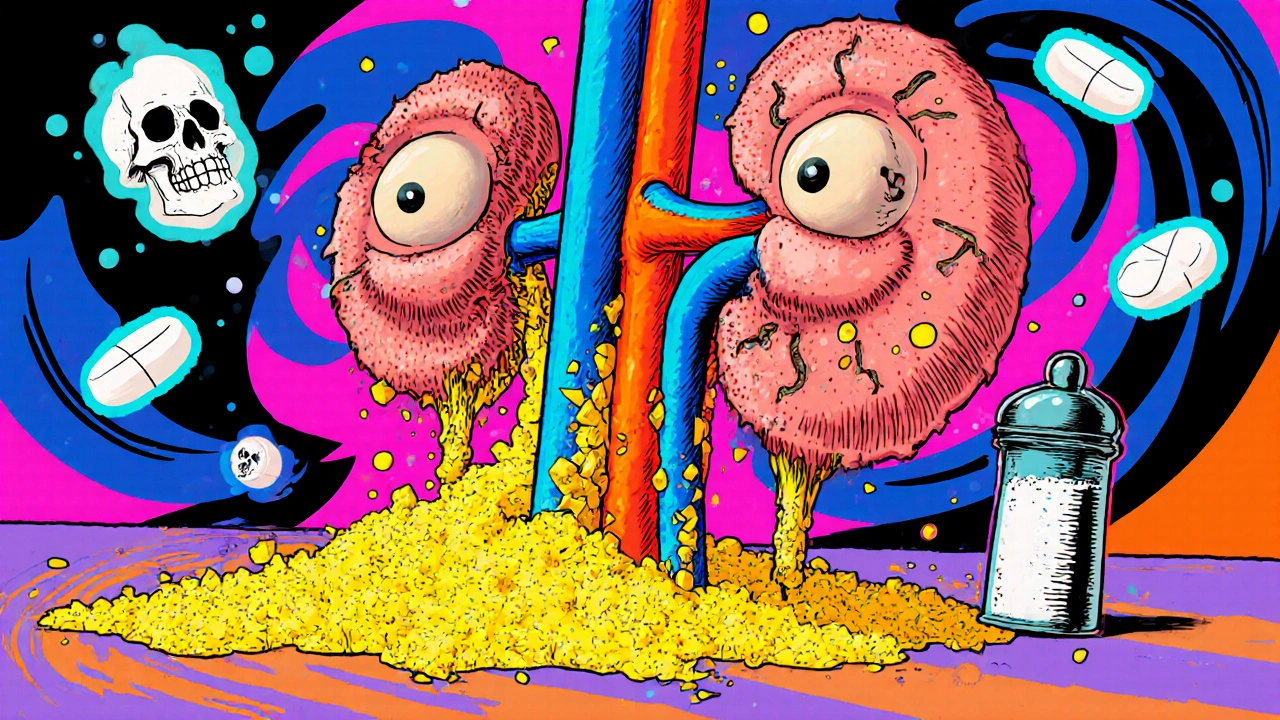
When your kidneys can’t filter waste and extra fluid properly, chronic kidney disease, a long-term condition where kidney function gradually declines leads to fluid overload, a dangerous buildup of excess fluid in the body. This isn’t just about feeling puffy—it’s a medical red flag. Your heart has to work harder, your blood pressure spikes, and swelling in your legs, lungs, or abdomen can turn life-threatening fast. People with CKD, chronic kidney disease, often progressing to end-stage renal failure are especially at risk, especially if they’re on dialysis or taking meds that hold onto sodium.
Fluid overload doesn’t happen overnight. It’s usually the result of drinking too much, eating salty foods, or not taking diuretics as prescribed. It’s also tied to mineral bone disorder in CKD, a complication where calcium, phosphate, and PTH levels go out of balance, which affects how your body handles fluids. If your kidneys aren’t removing sodium, your body holds onto water like a sponge. That’s why doctors push so hard on fluid restriction—even small changes, like cutting back on soups, ice, and soda, can make a real difference. Many patients don’t realize that a cup of ice counts as fluid, or that salty snacks make thirst worse, creating a cycle that’s hard to break.
What’s often missed is how fluid overload connects to other CKD complications. High fluid volume worsens heart strain, which is already a top cause of death in kidney patients. It also makes it harder to control blood pressure, which in turn damages your kidneys even more. That’s why managing fluid isn’t just about weight numbers—it’s about protecting your heart, your lungs, and your overall survival. The good news? Simple, daily habits—tracking intake, reading food labels, using smaller cups, and avoiding salty snacks—can cut hospital visits dramatically. You don’t need a PhD to do this. You just need to know what to watch for and how to act.
Below, you’ll find real, practical advice from posts that cover exactly these issues: how to track fluid intake without stress, why salt is your enemy, how diuretics work (and when they don’t), and what to ask your doctor when swelling won’t go away. These aren’t theory pieces—they’re tools used by people living with CKD every day.