Diuretics for Kidney Disease: What Works, What to Watch
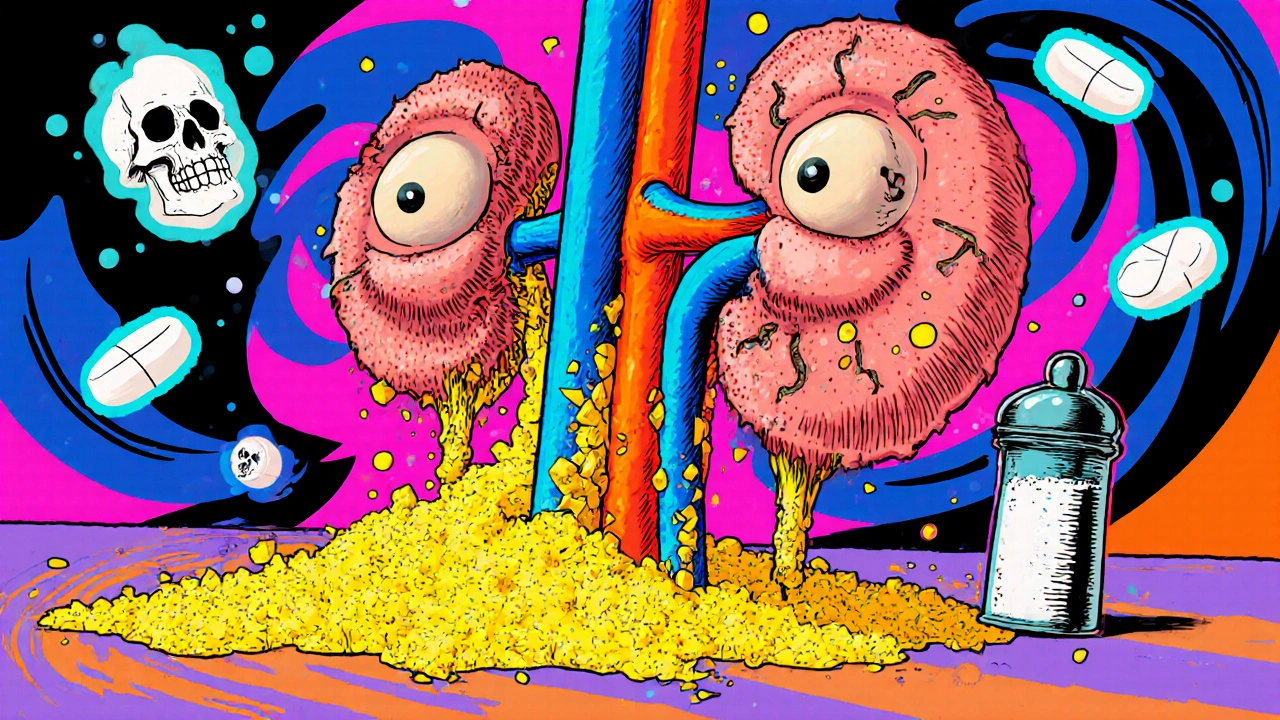
When your kidneys aren’t filtering fluid properly, diuretics for kidney disease, medications that help your body get rid of extra fluid through urine. Also known as water pills, they’re one of the most common tools doctors use to manage swelling, high blood pressure, and fluid overload in people with chronic kidney disease. But not all diuretics are the same — and picking the wrong one can make things worse.
There are three main types used in kidney disease: loop diuretics, stronger drugs like furosemide that work high up in the kidney’s filtering system, thiazide diuretics, milder options like hydrochlorothiazide that work lower down and are often used for early-stage disease or high blood pressure, and sometimes potassium-sparing diuretics, like spironolactone, which help reduce fluid without draining too much potassium. Each has a different strength, timing, and side effect profile. For example, loop diuretics are often needed when kidney function drops below 30%, while thiazides may stop working well once kidney damage gets advanced. You can’t just swap one for another — your doctor has to match the drug to your kidney’s current ability to process it.
It’s not just about taking the pill. Diuretics can cause electrolyte imbalances, low blood pressure, dizziness, or even kidney injury if you’re dehydrated. That’s why people on these meds often need regular blood tests to check sodium, potassium, and creatinine levels. If you’re also on blood pressure meds, statins, or NSAIDs like ibuprofen, the risk of interactions goes up. And if you’re losing too much fluid, your kidneys might start to shut down further — a vicious cycle that’s hard to reverse.
What you’ll find in the posts below isn’t just a list of drugs. It’s real-world advice on how these medications fit into the bigger picture of kidney health. You’ll see how they connect to mineral bone disorder, why fluid control matters for heart function, and how to talk to your pharmacist about side effects you might not even know to mention. Some posts even cover how insurance changes or generic availability can affect your access — because managing kidney disease isn’t just about the medicine, it’s about making sure you can actually get it, afford it, and stay safe while using it.