Palliative Care: What It Is, Who Needs It, and How It Helps
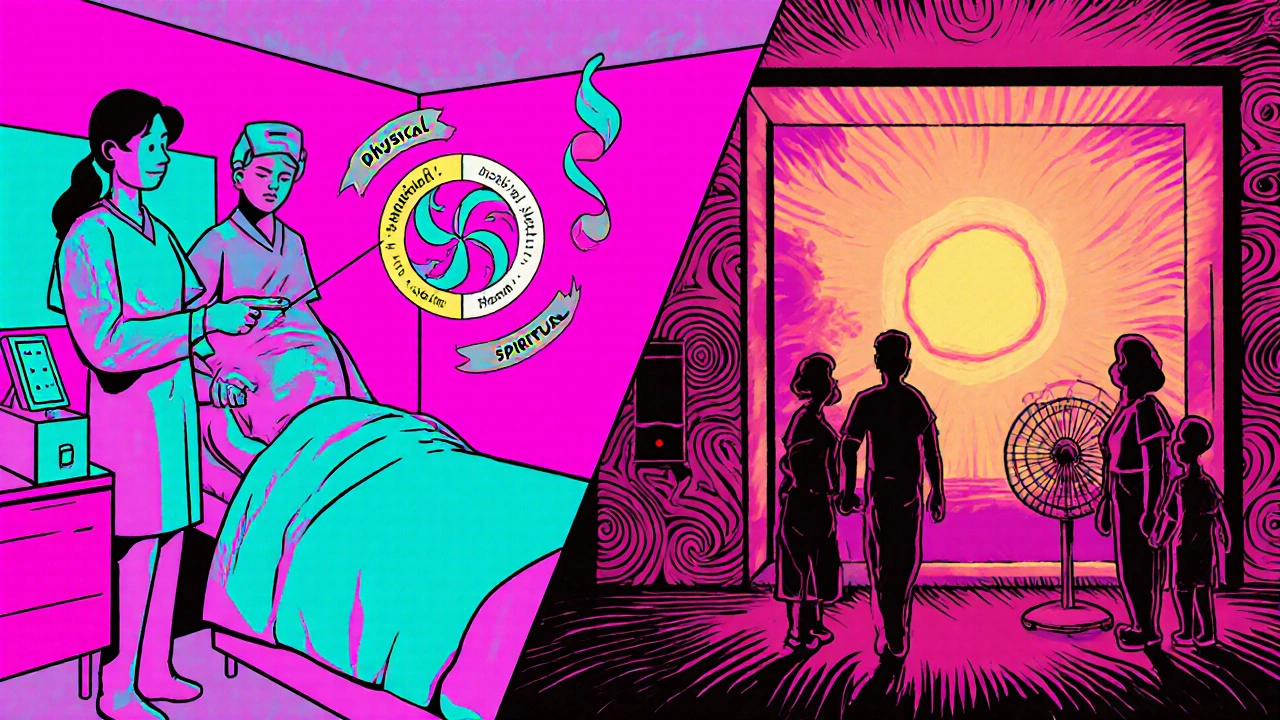
When someone is dealing with a serious illness like cancer, heart failure, or advanced dementia, the goal often shifts from curing to palliative care, a specialized approach focused on improving quality of life for patients and their families facing serious illness. Also known as comfort care, it’s not about giving up—it’s about making every day as meaningful and pain-free as possible. Many people confuse palliative care with hospice, but they’re not the same. Hospice is for those in the final months of life. Palliative care can start at diagnosis and happen alongside treatments like chemotherapy or surgery. It’s for anyone who needs help managing symptoms, no matter how long they have left.
At its core, palliative care is about pain management, the targeted use of medications and therapies to reduce physical discomfort from illness or treatment. It’s not just about pills—it includes breathing support, nausea control, anxiety relief, and even help with sleep. Symptom relief, the reduction of distressing physical and emotional effects caused by disease or treatment is the priority. A patient might be getting radiation for a tumor while also receiving palliative care to ease the fatigue and nausea from that same treatment. This isn’t an either-or situation—it’s both.
It’s not just the body that palliative care addresses. End-of-life care, the holistic support provided to patients and families as death approaches is part of the picture when the illness progresses. But even earlier, it helps with tough decisions: Should we keep trying aggressive treatments? What matters most to you now? Who should speak for you if you can’t? Palliative teams include doctors, nurses, social workers, and chaplains who talk through these questions without pushing any agenda. They listen. They help families understand what’s coming, so they’re not left guessing.
You don’t have to be old or terminally ill to benefit. Someone with chronic lung disease, advanced kidney failure, or even severe MS can get relief through palliative care. It’s not a last resort—it’s a better way to live with illness. And it’s not just for the patient. Family members get emotional support, guidance on caregiving, and help navigating insurance or home care options. This isn’t hospital-only care either. Many people get it at home, in nursing facilities, or even during outpatient visits.
The posts here don’t talk about palliative care directly, but they cover the conditions and medications that often lead people to need it. You’ll find guides on managing opioid-induced nausea with domperidone, treating chronic pain with gabapentin, handling side effects from cancer drugs, and using muscle relaxants like tizanidine for spasticity. These aren’t random topics—they’re pieces of the same puzzle. When someone is struggling with pain, nausea, anxiety, or sleep loss from a serious illness, these are the tools that palliative teams use every day.
What you’ll find below isn’t a list of theory—it’s real-world advice from people who’ve been there. Whether you’re a patient, a caregiver, or just trying to understand what palliative care really means, these posts give you the practical details you won’t get from a doctor’s office visit. No fluff. No jargon. Just what works, what doesn’t, and what to ask for next.